Tech Talk
Ex Vivo Confocal Microscopy: A Diagnostic Tool for Skin Malignancies
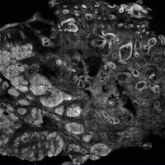
Confocal microscopy is an imaging tool that uses a laser system to image the skin noninvasively with cellular resolution. With both in vivo and ex...
All from the Department of Dermatology, Stanford University Medical Center, California. Dr. Nord also is from the Dermatology Service, VA Palo Alto Health Care System, California.
The authors report no conflict of interest.
This case was part of a presentation at the 8th Cosmetic Surgery Forum under the direction of Joel Schlessinger, MD; November 30-December 3, 2006; Las Vegas, Nevada. Dr. Sheu was a Top 10 Fellow and Resident Grant winner.
Correspondence: Kristin M. Nord, MD, VA Palo Alto Healthcare System, Dermatology Service, Mail Code 123, 3801 Miranda Ave, Palo Alto, CA 94304 (knord@stanford.edu).

Dermoscopy is used as an adjunct to clinical examination in the diagnosis of skin lesions, including melanoma. Videodermoscopy, which allows for the concurrent examination of dermoscopic features at high magnification by instructors and trainees, may serve as a useful educational tool during bedside instruction. This article presents images of common cutaneous lesions taken with a standard optical dermatoscope and a videodermatoscope to highlight the potential educational advantages conferred by videodermoscopy.
Resident Pearl
Dermoscopy, or the noninvasive in vivo examination of the epidermis and superficial dermis using magnification, facilitates the diagnosis of pigmented and nonpigmented skin lesions.1 Despite the benefit of dermoscopy in making early and accurate diagnoses of potentially life-limiting skin cancers, only 48% of dermatologists in the United States use dermoscopy in their practices.2 The most commonly cited reason for not using dermoscopy is lack of training.
Although the use of dermoscopy is associated with younger age and more recent graduation from residency compared to nonusers, dermatology resident physicians continue to receive limited training in dermoscopy.2 In a survey of 139 dermatology chief residents, 48% were not satisfied with the dermoscopy training that they had received during residency. Residents who received bedside instruction in dermoscopy reported greater satisfaction with their dermoscopy training compared to those who did not receive bedside instruction.3 This article provides a brief comparison of standard dermoscopy versus videodermoscopy for the instruction of trainees on common dermatologic diagnoses.
Standard optical dermatoscopes used for patient care and educational purposes typically incorporate 10-fold magnification and permit examination by a single viewer through a lens. With standard dermatoscopes, bedside dermoscopy instruction consists of the independent sequential viewing of skin lesions by instructors and trainees. Trainees must independently search for dermoscopic features noted by the instructor, which may be difficult for novice users. Simultaneous viewing of lesions would allow instructors to clearly indicate in real time pertinent dermoscopic features to their trainees.
Videodermatoscopes facilitate the simultaneous examination of cutaneous lesions by projecting the dermoscopic image onto a digital screen. Furthermore, these devices can incorporate magnifications of up to 200-fold or greater. In recent years, research pertaining to videodermoscopy has focused on the high magnification capabilities of these devices, specifically dermoscopic features that are visualized at magnifications greater than 10-fold, including the light brown nests of basal cell carcinomas that are seen at 50- to 70-fold magnification, twisted red capillary loops seen in active scalp psoriasis at 50-fold magnification, and longitudinal white indentations seen on nail plates affected by onychomycosis at 20-fold magnification.4-6 The potential value of videodermoscopy in medical education lies not only in the high magnification potential, which may make subtle dermoscopic findings more apparent to novice dermoscopists, but also in the ability to facilitate simultaneous dermoscopic examinations by instructors and trainees.
To illustrate the educational potential of videodermoscopy, images taken with a standard dermatoscope at 10-fold magnification are presented with videodermoscopic images taken at magnifications ranging from 60- to 185-fold (Figures 1–3). These examples demonstrate the potential for videodermoscopy to facilitate the visualization of subtle dermoscopic features by novice dermoscopists, relating to both the enhanced magnification potential and the potential for simultaneous rather than sequential examination.
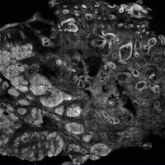
Confocal microscopy is an imaging tool that uses a laser system to image the skin noninvasively with cellular resolution. With both in vivo and ex...

Dr. Anthony Rossi discusses the use of ex vivo confocal microscopy to aid in the diagnosis of skin disease and skin tumors. He explains how this...
Previous studies have demonstrated incomplete sunscreen self-application to various facial regions in cosmetic surgery patients, but there is no...
