AMSTERDAM – The new systemic lupus erythematosus classification criteria of the American College of Rheumatology and the European League Against Rheumatism are based on a point system that will produce a “paradigm shift” in how the disease gets studied going forward, said Sindhu Johnson, MD, while presenting the latest version of the newly revised classification scheme at the European Congress of Rheumatology.
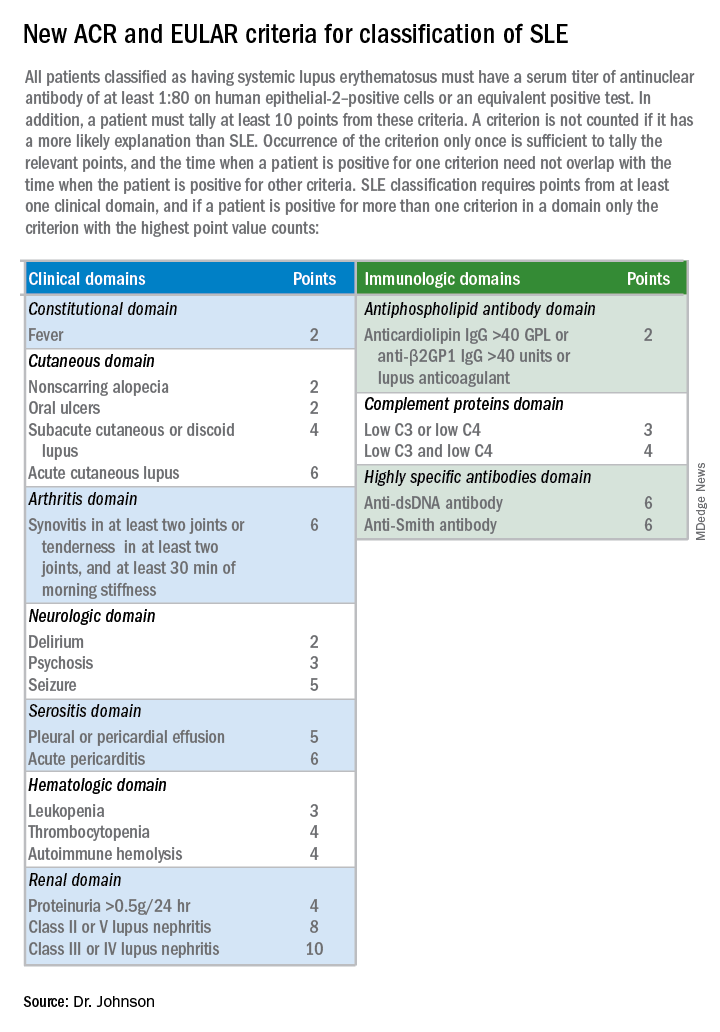
Until now, classification of systemic lupus erythematosus (SLE) was a yes-or-no decision, based on whether the patient had a minimum number of characteristic signs or symptoms. The new criteria, which are on track for formal endorsement before the end of 2018 by the two medical societies that sponsored the revision, instead use a point system that gives varying weight to each of the 22 criteria. A patient needs to score at least 10 points from these criteria, and all patients classified with SLE also must have an antinuclear antibody (ANA) titer of at least 1:80 on HEp-2 cells or an equivalent positive test. This means that the criteria also can define patients who just miss classification with SLE by meeting the ANA standard and by tallying 8 or 9 points, and the criteria also identify patients who far exceed the classification threshold by having the requisite ANA plus racking up as many as, perhaps, 20 or 30 points.
“This is a real research opportunity,” to follow patients who fall just short with 8 or 9 points to assess their longer-term prognosis, as well as to study whether “higher scores mean a higher risk for developing a bad outcome,” said Dr. Johnson , a rheumatologist at the University of Toronto and director of the Toronto Scleroderma Program. Other areas for future research with the new criteria include seeing how they work in various SLE subgroups, such as patients with renal-predominant disease or skin-predominant disease, and also seeing how they work in various ethnic populations.
Dr. Johnson acknowledged the importance the new classification criteria will have for diagnosing SLE in routine practice, even though the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) both stress that the classification criteria are intended only for research and not for diagnosis.“Diagnosis of lupus still falls within the realm of the treating physician,” but the classification criteria “inform our concept of the disease,” Dr. Johnson said in a video interview. “The new criteria allow for a shift in the way we think of the disease.”
For example, for the first time, the new criteria includes fever as a classification criterion, which receives 2 points if an infectious or other non-SLE cause can be discounted. Fever has recently been identified as a marker of early-stage SLE in at least some patients, and its addition to the classification criteria “adds a new dimension to how we think about the disease and allows us to distinguish early disease from mimicking diseases,” she explained. At the other end of the classification spectrum, a finding of class III or IV lupus nephritis on renal biopsy receives 10 points, and hence, this one finding plus having a high enough level of ANA leads to SLE classification regardless of whether the patient has any other signs or symptoms of the disease.
That’s because “85% of our experts said that they would feel confident classifying a patient as having lupus based only on a renal biopsy” and ANA positivity, said Dr. Johnson, who served as the ACR-appointed cochair of the criteria-writing panel along with a cochair selected by EULAR, Martin Aringer, MD, PhD , of the Technical University of Dresden (Germany). She cautioned that other levels of lupus nephritis, class II or V, confer only 8 points to the classification and so by themselves are not enough to label a person as having lupus.
During her presentation, Dr. Johnson cited the high levels of sensitivity and specificity that the new classification criteria demonstrated in a validation cohort of more than 1,000 cases and controls. In the validation analysis, the new criteria had a sensitivity of 96.12% and specificity of 94.43% for classifying SLE, giving the new criteria a better result on both these measures than either the 1997 ACR criteria ( Arthritis Rheum. 1997 Sept;40[9]:1725 ) or the 2012 Systemic Lupus International Collaborating Clinics criteria ( Arthritis Rheum. 2012 Aug;64[8]:2677-86 ).
The 22 criteria cluster into seven separate clinical domains and three different immunologic domains. The point values assigned to each criterion range from 2 to 10 points.
Dr. Johnson had no disclosures.