To the Editor:
A 60-year-old woman with a history of lymphoma presented to the emergency department for evaluation of intermittent diarrhea and vomiting of 2 weeks’ duration. On presentation, a rather large dressing covering the entire right half of the face was noted. Removal of the bandage revealed a necrotic, extensively destructive, right-sided facial lesion with a fully exposed ocular globe (Figure 1). The patient lived alone and was accompanied by a neighbor, who disclosed that the lesion had been neglected and enlarged over the last 15 years. Moreover, the neighbor reported that the patient had recently experienced several episodes of vertigo and frequent falls.
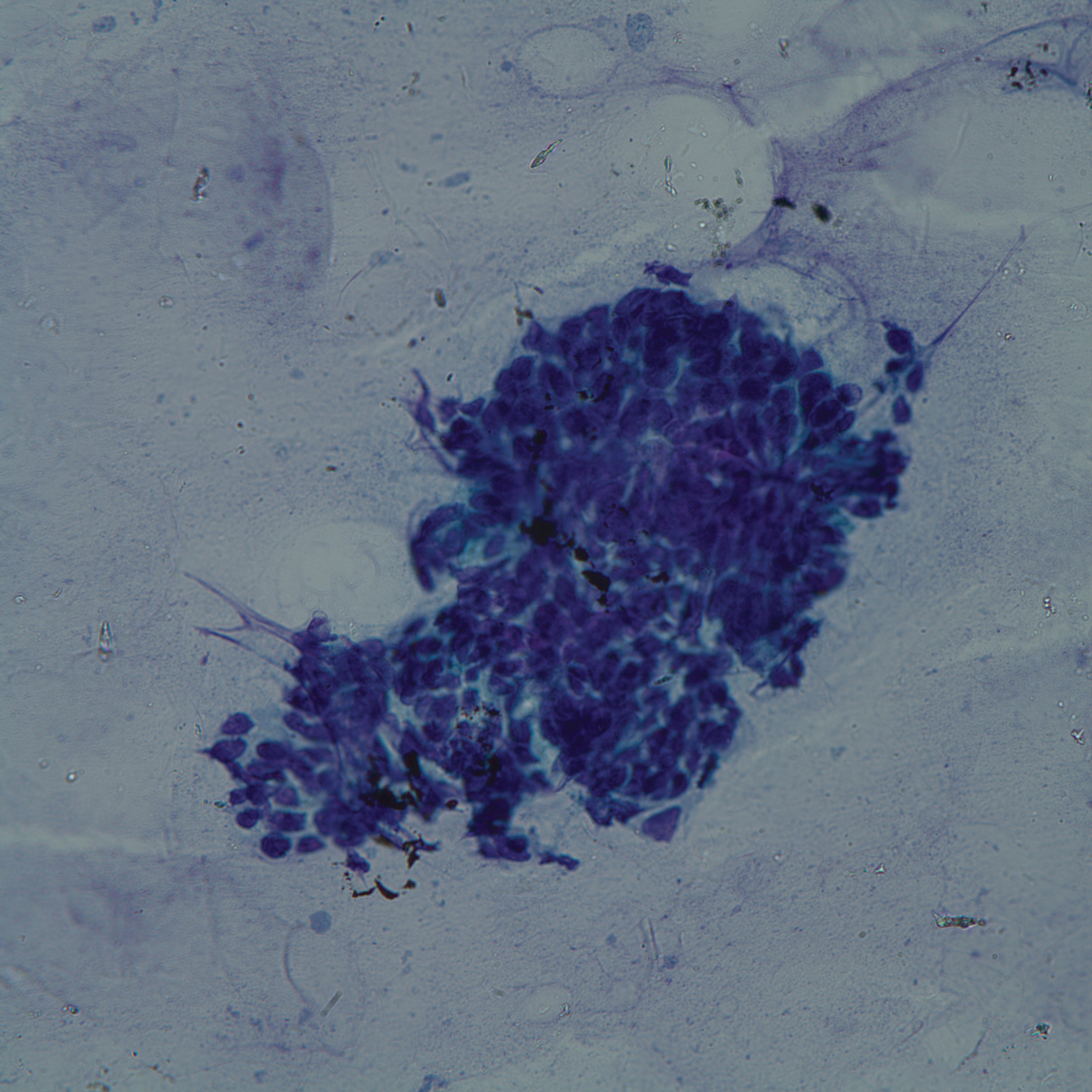
On admission to the hospital, dermatology was consulted and initial workup included computed tomography (CT) scan of the head and maxillofacial region, which showed a destructive process involving the right frontotemporal bone, maxillofacial region, sphenoid, and skull base with exposure of intracranial contents (Figure 2). An aggressive wound care regimen was instituted. Biopsy of the wound margin revealed nodular and focally infiltrative basal cell carcinoma (BCC) (Figure 3). Culture of the necrotic bone grew Rhizopus, a causative organism of mucormycosis, and the patient was treated with posaconazole. A CT scan of the chest and abdomen showed multiple bilateral pulmonary nodules and necrotic lymph nodes in the left hilum and left axilla. The patient refused bronchoscopy to further evaluate the pulmonary nodules. Ultrasound-guided biopsy of the left axillarylymph node revealed metastatic disease (Figure 4).