It has been more than 10 years since Congress passed the HITECH Act to jump start the adoption of electronic health records. And yet interoperability, the key to making their adoption meaningful, remains an elusive target.
Members of the Senate Health, Education, Labor, and Pensions Committee questioned whether attempts to regulate interoperability – and health IT in general – are doing more harm than good in terms of creating a truly interoperable environment.
A key concern raised during a May 7 hearing examining the implementation of the health IT provisions of the 21st Century Cures Act (H.R. 34), signed into law in December 2016, was that the slow speed of government regulatory action simply cannot keep pace with innovation.
“In 2016, my question to a panel like this was, ‘How the hell are you going to do this?’ I think what you’ve heard is different variations of that going around the room,” Sen. Richard Burr (R-N.C) said. “The difference is we’re in 2019 and this is a discussion that we started in 2013 about how do we get systems to talk to other systems.”
“Here is my problem,” he continued, noting that between 2013 and 2019, “technology has exploded. It runs at an unbelievable pace. And here we are trying to set standards and set architecture of software ... that 12 months from now is going to be obsolete because that’s how fast technology is changing.”
Sen. Burr added that the problem is that government can’t regulate fast enough. “Our problem is we can’t get rules through when the technology that we are applying it to is in existence. By the time we get a rule through, technology’s changed, and it may or may not apply.”
Donald Rucker, MD, national coordinator for health information technology at the Health & Human Services department, testified that the current app marketplace is “stable” and “the entire point of what we are doing jointly is to allow these apps in the market economy to incorporate patient’s medical data into that.”
Centers for Medicare & Medicaid Services Chief Medical Officer Kate Goodrich, MD, agreed.
“I would absolutely agree with Don that the timing is really right for this because of where the state of play is with the standards, and I think it’s a good time to take advantage of that and move the field forward,” she testified at the hearing.
The Office of the National Coordinator for Health IT recently issued a proposed rule related to interoperability. The CMS has issued a concurrent proposed rule, also related to interoperability.
Sen. Burr, however, was not moved by these assurances.
“I am probably no less convinced that we are going to get to the finish line today than I was in 2016, though the tools that we have are much better,” he said, telling an anecdote about how providers and insurers took the initiative to improve the outcomes of diabetes patients without any prompting from legislative or regulatory action.
“It seems to me that that’s the most appropriate first place to go, is to create an incentive for the providers,” he said. “It is to their financial benefit to do that.”
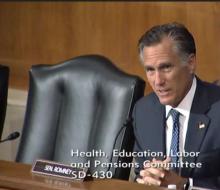
Sen. Mitt Romney (R-Utah) also expressed doubt as to whether the goal of interoperability was achievable.
“I wonder exactly whether it is conceivable for us to achieve standards that will allow systems to talk to each other from one hospital system, for instance, to another provider, or whether that’s frankly a bridge too far at this stage,” he said.
Dr. Rucker acknowledged that there is “plenty of room for skepticism,” but he said that the goals of interoperability in health care are achieved broadly across most sectors in the economy today, and it’s about customizing what already works in the marketplace to the needs of the health care environment.
Dr. Goodrich agreed, noting that, in her time as a practicing physician, she has seen advances in the amount of data that can be transfered electronically.
“There is reason for optimism,” she said. “So, yes, plenty of room for skepticism, but also more optimism than probably any of us would have had a couple of years ago.”