Metacognition is already embedded in the fabric of the physician-patient interaction.33,34 The complex interplay of the physician-patient interview, patient examination, and integration of physical as well as ancillary data requires higher-order thinking and the ability to parse out that thinking successfully. As a concrete example, coming to a diagnosis requires thinking about what has been presented during the physician-patient interaction and considering what supports and suggests the disease while a list of potential differential diagnosis alternatives is being generated. Physicians are trained to apply this clinical reasoning approach to their patient care.
Conversely, although communication skills are a key component of doctoring,38 both between physician and patient as well as among other colleagues and staff, many physicians have never received formal training in communication skills,26,32,39 though it is now an integral part of medical school curricula.40 When such training is mandatory, less than 1% of physicians continue to believe that there was no benefit, even from a single 8-hour communications skills training session.41 Communication cannot be taught comprehensively in 8 hours; thus, the benefit of such training may be the end result of metacognition and increased self-awareness (Table 1).42,43
Building Relationship-Centered Care Through Metacognitive Attention
Metacognition as manifested by such self-awareness can build relationship-centered care.4 Self-awareness can be taught through mentorship or role models.44 Journaling,40 meditation, and appreciation of beauty and the arts45 can contribute, as well as more formal training programs,32,38,42 as offered by the Academy of Communication in Healthcare. Creating opportunities for patient empowerment also supports relationship-centered care, as does applying knowledge of implicit bias.46
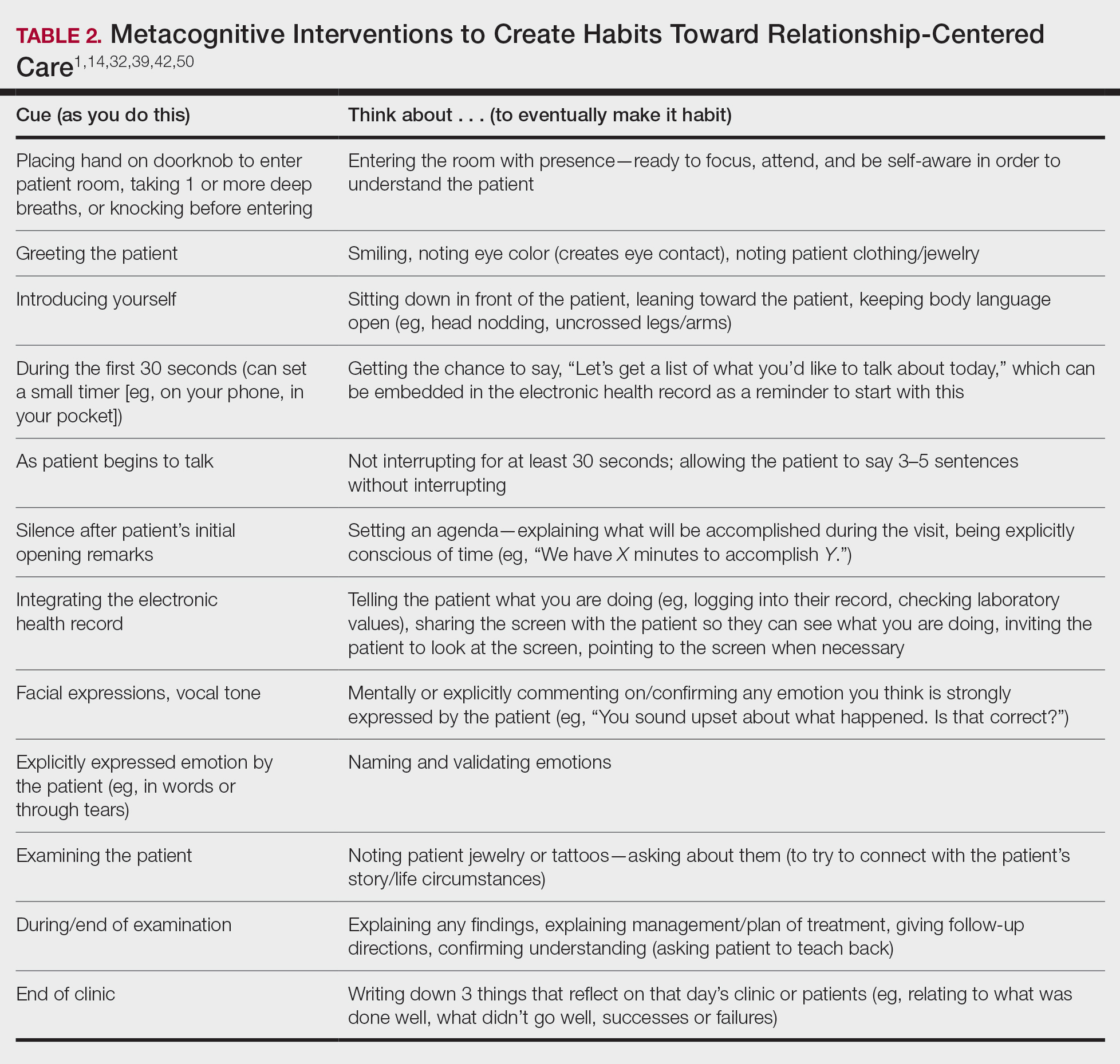
Even without formal training, relationship-centered care can be built through attention to cues9—visual (eg, sitting down, other body language),47,48 auditory (eg, knocking, language, tone, conversational flow),48,49 and emotional (eg, clinical empathy, emotional intelligence)(Table 2). Such attention is familiar to everyone, not just physicians or patients, through interactions outside of health care; inattention may be due to the hidden curriculum or culture of medicine40 as well as real-time changes, such as the introduction of the electronic health record.51 Inattention to these cues also may be a result of context-specific knowledge, in which a physician’s real-life communication skills are not applied to the unique context of patient care.
Although the theoretical foundation of relationship-centered care is relatively complex,9 a simple formula that has improved patient experience is “The Big 3,” which entails (1) simply knocking before entering the examination room, (2) sitting, and (3) asking, “What is your main concern?”30 Another relatively simple technique would be to involve the patient with the electronic health record by sharing the screen with them.52 Learning about narrative medicine and developing skills to appreciate each patient’s story is another method to increase relationship-centered care,40,53 as is emotional intelligence.54 These interventions are simple to implement, and good relationship-centered care will save time, help manage patient visits more effectively, and aid in avoiding the urgent new concern that the patient adds at the end of the visit.55 The positive effect of these different interventions highlights that small changes (Table 2) can shift the prevailing culture of medicine to become more relationship centered.56
Metacognitive Attention Can Generate Habit
Taking metacognition a step further, these small interventions can become habit11,14,39 through self-awareness, deliberate practice, and feedback.43 Habit is generated by linking a given intervention to another defined cue. For example, placing a hand on a doorknob to enter an examination room can be the cue to generate a habit of entering with presence.14 Alternatively, before entering an examination room, taking 3 deep breaths can be the cue to trigger presence.14 Habits can be created in just 3 weeks,57 and other proposed cues to generate habits toward relationship-centered care are listed in Table 2. By creating habit through metacognitive attention, relationship-centered care will become something that happens subconsciously without further burdening physicians with another task. Asking patients for permission to record video of an interaction also can create opportunities for self-awareness and self-evaluation through rewatching the video.58
Final Thoughts
Physicians already have the tools to create relationship-centered care in physician-patient interactions. A critical mental shift is to develop habits and apply thinking patterns toward understanding and responding appropriately to patients of all ethnicities and their emotions in the physician-patient interaction. This shift is aided by metacognitive awareness (Table 1) and the development of useful habits (Table 2).