The Diagnosis: Atrophic Lupus Erythematosus
Cutaneous lupus erythematosus is divided into acute, subacute, and chronic cutaneous lupus erythematosus (CCLE). There are more than 20 subtypes of CCLE mentioned in the literature including atrophic lupus erythematosus (ALE).1 The most typical presentation is CCLE with discoid lesions. Most commonly, discoid CCLE is an entirely cutaneous process without systemic involvement.Discoid lesions appear as scaly red macules or papules primarily on the face and scalp.2 They may evolve into hyperkeratotic plaques with irregular hyperpigmented borders and develop a central hypopigmented depression with atrophy and scarring.2,3 Discoid CCLE has a female predominance and commonly occurs between 20 and 30 years of age. Triggers of discoid lesions include UV exposure, trauma, and infection.2
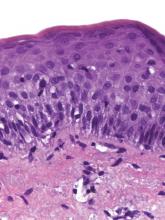
Our case of multiple atrophic plaques of the face, scalp, trunk, and upper extremities demonstrated a diagnostic challenge. Our patient presented with atrophic facial plaques, which are not typical of discoid lesions of CCLE. Our patient’s findings appeared clinically similar to acne scarring or atrophoderma. Histology showed common features of CCLE, including basal liquefactive degeneration, thickening of the basement membrane zone, increased melanin, and a lymphocytic inflammatory infiltrate (Figure).2,3 There was no evidence of hyperkeratosis, which often is seen in discoid lesions of CCLE.
Clinicopathologically, our case was consistent with ALE. A review of the literature revealed similar cases documented by Christianson and Mitchell4 in 1969; they described annular atrophic plaques of the skin of unknown diagnostic classification. Chorzelski et al5 reiterated the difficulty of defining diagnostically similar atrophic plaques of the face showing histopathologic features consistent with lupus and suggested these cases may represent an uncharacteristic presentation of discoid lupus erythematosus. Our patient demonstrated this rare subtype of discoid lupus erythematosus, known as ALE. There are few reports in the literature of ALE; thus we have managed our patient similar to other CCLE patients. Management of CCLE patients includes strict sun protection. Treatment options include corticosteroids, calcineurin inhibitors, antimalarial agents, and thalidomide.2 Our patient started using tacrolimus ointment 0.1% daily and hydroxychloroquine 200 mg twice daily. She also was practicing strict photoprotection. The patient was lost to follow-up. Topical steroids are not an option in ALE. It is important for dermatologists to recognize this rare variant of CCLE to prevent disfigurement.