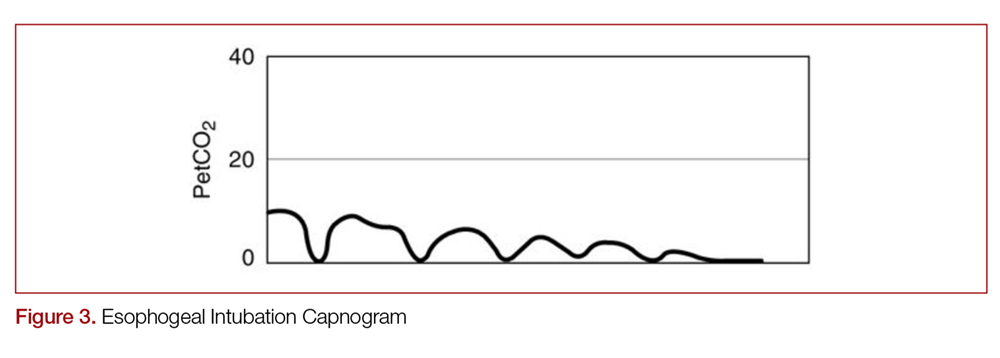
With quantitative capnography, obtaining the typical box-waveform on the capnogram reflects endotracheal intubation. In comparison, a flat capnogram is more indicative of an esophageal intubation (Figure 3).10 While other things may cause this waveform, such as technical malfunction or complete airway obstruction distal to the tube, tube placement confirmation to rule out esophageal intubation would be the first step to troubleshooting this waveform. In addition, if the ETT is placed in the hypopharynx above the vocal cords, the waveform may initially appear appropriate but will likely become erratic appearing over time.10
Quantitative capnography does have some limitations. For example, a main-stem bronchus intubation would still likely demonstrate normal-appearing capnography, so secondary strategies and a confirmatory chest x-ray are still indicated. False-negative ETCO2 readings can occur in low CO2 elimination states, such as cardiac arrest, pulmonary embolus, or pulmonary edema, while false-positives can theoretically occur after ingestion of large amounts of carbonated liquids or contamination of the sensor with stomach contents or acidic drugs.10 However, many of these misleading results can be caught by simply checking for an appropriate waveform.
Cardiac Arrest
Capnography has numerous uses in the monitoring, management, and prognostication of intubated patients in cardiac arrest.1,3,4,10,14 Under normal conditions, EtCO2 is 35-40 mm Hg. While the body still makes CO2 during cardiac arrest, it will not reach the alveoli without circulating blood.10 Without CPR, CO2 accumulates peripherally and won’t reach the lungs, causing EtCO2 to approach zero. This means that EtCO2 correlates directly with cardiac output during CPR, as long as ventilation remains constant.
This means the effectiveness of cardiac chest compression can be assessed in intubated patients using EtCO2, with higher values during CPR correlated with increased return of spontaneous circulation (ROSC) and survival.14-18 Using EtCO2 monitoring during cardiac arrest may improve outcomes,19 and the American Heart Association (AHA) recommends monitoring capnography during cardiac arrest to assess compression efficacy.10,20 EtCO2 >20 mm Hg is considered optimal, while EtCO2 <10-15 mm Hg is considered suboptimal.4,10,16 In a recent meta-analysis, the average EtCO2 was 13.1 mm Hg in those who did not obtain ROSC, compared to 25.8 mm Hg in those who did.21 As such, goal EtCO2 for effective compressions may be even higher in future recommendations. If EtCO2 is low, either compression technique should be improved or a different operator should do compressions. Every 1 cm increase in depth will increase EtCO2 by approximately 1.4 mm Hg.16 Interestingly, compression rate is not a significant predictor of EtCO2 over the dynamic range of chest compression delivery.16
An abrupt increase in EtCO2 is an early indicator of ROSC.10,14-16,22,23 A return of a perfusing rhythm will increase cardiac output. This allows for accumulated peripheral CO2 to reach the lungs, subsequently causing a rapid rise in EtCO2.24 It is important to note that when it comes to evaluating for ROSC, the actual numbers are less important than the change from pre- to post-ROSC. Providers should look for a jump of at least 10 mm Hg on capnometry.4 Nevertheless, an abrupt rise in EtCO2 is a non-sensitive marker for ROSC (33%, 95% CI 22-47% in one multicenter cross-sectional study), meaning that the lack of an abrupt rise of EtCO2 may not necessarily mean a lack of ROSC.23