The EtCO2 level may help guide decision-making in assessing whether continued resuscitation in cardiac arrest is futile. Values <10 mm Hg after 20 minutes of active resuscitation have consistently demonstrated minimal chance of survival.17,25,26 In one study, an EtCO2 of <10 mm Hg at 20 minutes had a sensitivity, specificity, PPV, and NPV of 100% for death in PEA arrest.17 However, determination of the specific EtCO2 cutoff and the timing is still an area of research with a final consensus pending.17,18,25-30 One recent study suggested that even 3 min with EtCO2 <10 mm Hg could be an appropriate cutoff to cease resuscitation efforts.27
Unfortunately, there is a large amount of heterogeneity in the available literature using capnography to assess for ROSC and in guiding resuscitation efforts. EtCO2 should not be used as the only factor in the determination to cease resuscitation. In addition, the AHA recommends that EtCO2 for prognostication should be limited to intubated patients only.20
It is important to note that while cardiac output is the largest factor for EtCO2 in arrest, other physiologic and iatrogenic causes may affect EtCO2 during resuscitation. For example, there is considerable variation in EtCO2 with changes in ventilation rate.4 Measured CO2 may be significantly lower with manual instead of mechanical ventilation, likely due to over-ventilation that not only reduces alveolar CO2 but also causes excess intra-thoracic pressure, reducing venous return.21 For these reasons, use caution when using EtCO2 during manual ventilation of an intubated patient in cardiac arrest. In addition, administration of epinephrine may cause a small decrease in EtCO2, although the effect may vary for each individual.10,31 Sodium bicarbonate can also cause a transient increase in CO2 due to its conversion into CO2 and H2O.10
Procedural Sedation
Capnography is being used with increasing frequency to monitor patients during procedural sedation; it is now considered standard of care in many settings.32 Although rare, hypoventilation is a risk of procedural sedation.33 Typically, respiratory depression during procedural sedation is diagnosed with non-invasive pulse oximetry and visual inspection.34 However, capnography has been shown to identify respiratory depression, airway obstruction, apnea, and laryngospasm earlier than pulse oximetry, allowing the provider to intervene quicker.34,35 Unlike pulse oximetry, the capnogram also remains stable during patient motion and is reliable in low-perfusion states.36
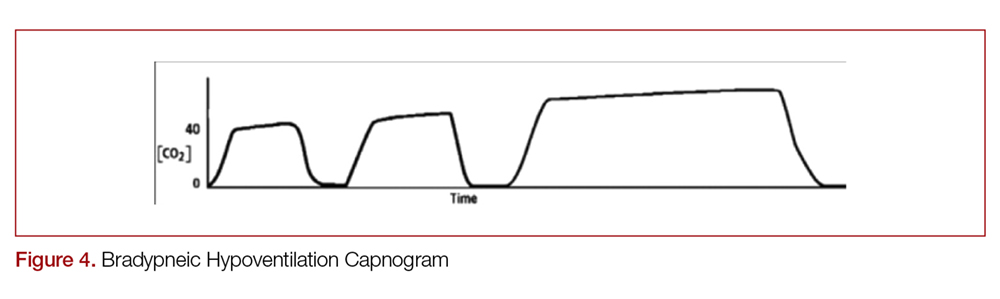
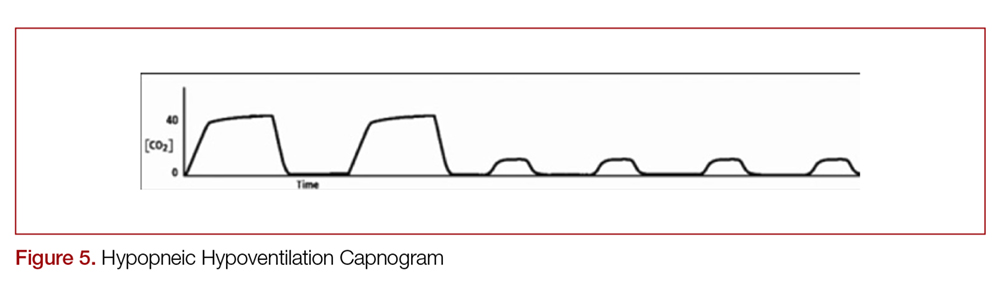
There are two distinct types of hypoventilation detected by capnography. Bradypneic hypoventilation (type 1), which is characterized by a decreased respiratory rate, results in a decreased expiratory time and a subsequent rise in EtCO2.36 This is depicted on capnography by a high EtCO2 and longer waveform, and is commonly observed after oversedation with opioids (Figure 4).36 In contrast, hypopneic hypoventilation (type 2) occurs with low tidal volumes but a normal respiratory rate.36 Type 2 is graphically represented by a suddenly lower ETCO2 with otherwise normal waveform and occurs most commonly with sedative-hypnotic drugs (Figure 5).36 Seeing either type during procedural sedation should alert the clinician to assess for airway obstruction, consider supplemental oxygen, cease drug administration or reduce dosing, and consider reversal if appropriate.36