2. Fanucci E, Fiaschetti V, Rotili A, Floris R, Simonetti G. Whole body 16-row multislice CT in emergency room: Effects of different protocols on scanning time, image quality and radiation exposure. Emerg Radiol. 2007;13(5):251-257.
3. Nguyen D, Platon A, Shanmuganathan K, Mirvis SE, Becker CD, Poletti PA. Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. AJR Am J Roentgenol. 2009;192(1):3-10.
4. Huber-Wagner S, Biberthaler P, Haberle S, et al. Whole-body CT in haemodynamically unstable severely injured patients – A retrospective, multicentre study. PLoS One. 2013;8(7):e68880.
5. Salim A, Sangthong B, Martin M, Brown C, Plurad D, Demetriades D. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: Results of a prospective study. Arch Surg. 2006;141(5):468-473; discussion 473-475.
6. Stengel D, Frank M, Matthes G, et al. Primary pan-computed tomography for blunt multiple trauma: Can the whole be better than its parts? Injury. 2009;40 Suppl 4:S36-S46.
7. Sierink JC, Saltzherr TP, Beenen LF, et al. A multicenter, randomized controlled trial of immediate total-body CT scanning in trauma patients (REACT-2). BMC Emerg Med. 2012;12:4-227X-12-4.
Obstructed Views: Imaging in Urinary Tract Obstruction
Lily M. Belfi, MD
Dr Belfi is an assistant professor of radiology at Weill Cornell Medical College in New York City and an assistant attending radiologist at New York-Presbyterian Hospital/Weill Cornell Medical Center.
Urinary tract (UT) obstruction is one of the most common indications for genitourinary (GU) imaging in the ED. Until recently, diagnosis was made using intravenous (IV) pyelography. Today, improved imaging modalities, such as noncontrast computed tomography (CT), computed tomography urography (CTU), magnetic resonance urography (MRU), and magnetic resonance imaging (MRI), are available to better visualize and evaluate the underlying causes of obstruction.
Noncontrast Computed Tomography
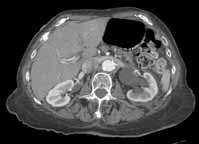
Figure 1. Axial and coronal noncontrast pelvic computed tomography scans (A and B) of a 90-year-old woman with left flank pain shows hydronephrosis (white arrow) and the left ureter extending into the sciatic notch (red arrow). |
Noncontrast CT of the abdomen and pelvis is the imaging study of choice in evaluating acute GU obstruction, particularly when there is clinical suspicion of stone disease. CT is extremely sensitive and specific in detecting renal calculi and provides information about stone burden, size, location, and composition. In addition to renal calculi, noncontrast CT is also useful in identifying other, less common causes of UT obstruction such as ureteral herniation, which can occur in the inguinal, femoral, or sciatic region and result in acute obstruction. Patients with neuromuscular disorders that cause piriformis muscle atrophy (eg, multiple sclerosis) may be predisposed to ureteral sciatic herniation. CT reconstructions in the coronal plane are useful in detecting this condition (Figure 1).
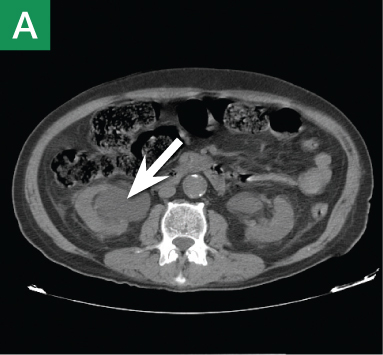
| Figure 2. Coronal noncontrast pelvic computed tomography (CT ) scan (A) of a 25-year-old woman with right flank pain reveals a duplicated collecting system (white arrows). Axial CT of the urinary bladder (B) reveals an obstructing ureterocele (red arrow). |
Reconstructed CT images can also reveal underlying congenital abnormalities that make a patient susceptible to obstruction. For example, CT can reveal the presence of a duplicated collecting system, which is often accompanied by an obstructing ureterocele associated with the upper pole moiety (Figure 2).
Computed Tomography Urography
| Figure 3. Computed tomography urography images (A and B) reveal "fish-hook" ureter (white arrows) classically seen in patients with with retrocaval ureter. | |||
Other types of congenital anomalies may require additional imaging with CTU, in which IV iodinated contrast media is administered for increased sensitivity and visualization. For instance, patients with a retrocaval ureter often present with GU obstruction and hematuria; the classic “fish-hook” or “sickle-shaped” deformity of the ureter characterizing this disease is best visualized on CTU as the ureter is well-opacified by excreted contrast (Figure 3).
Magnetic Resonance Urography and Magnetic Resonance Imaging
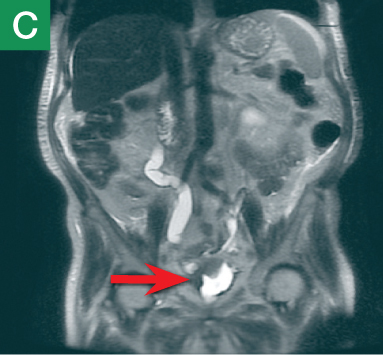
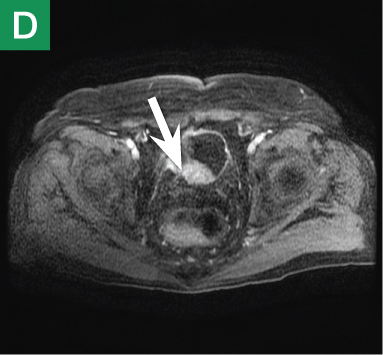
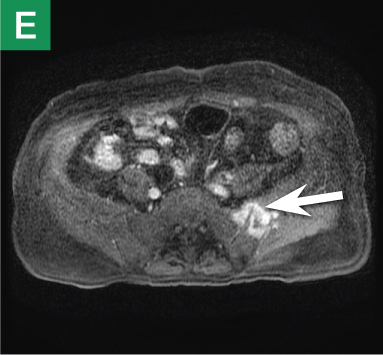
MRU and MRI are alternative modalities to CTU for patients in whom iodinated CT contrast is contraindicated or in cases where the avoidance of radiation exposure is indicated (eg, pregnant and pediatric patients). MRI and MRU are especially useful in further characterizing obstructive lesions in the GU tract. While initial noncontrast CT may suggest soft-tissue lesions within the ureter or urinary bladder, follow-up MRI clearly delineates the condition, helping clinicians quantify the extent of tumor involvement and determine disease stage (Figure 4). Pelvic MRI is also an essential tool in identifying causes of bladder outlet obstruction, especially in those involving the prostate gland (Figure 5).
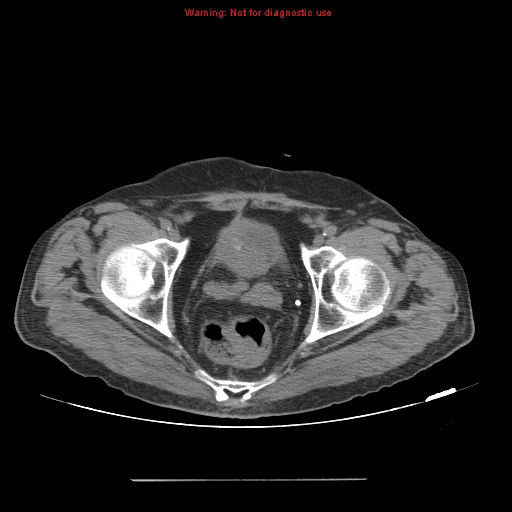
Figure 4. Noncontrast pelvic computed tomography images (A and B) of a 72-year-old man with flank pain and difficulty voiding reveal hydronephrosis (white arrow) and bladder mass (red arrow). Magnetic resonance urography (C) further visualizes the bladder mass (red arrow), and postcontrast magnetic resonance images (D and E) show the extent of the tumor (red arrow) as well as a metastatic lesion (white arrow). | ||||