Conclusion
| Figure 5. Noncontrast pelvic computed tomography images (A and B) of a 73-yearold man with pelvic pain demonstrate bilateral hydronephrosis. (white arrows) and a large mass in the expected location of the prostate (red arrow). Further evaluation of the large heterogenous mass with pelvic magnetic resonance imaging (C) reveals prostate carcinoma (red arrows). | |||||
Based on its sensitivity in detecting both common and uncommon causes of obstruction, noncontrast abdominal and pelvic CT is an excellent first-line imaging choice for evaluating patients presenting to the ED with UT obstruction. Moreover, noncontrast CT also helps guide clinicians in determining which, if any, additional studies with CTU, MRU, and/or MRI are warranted.
Sound Advice: Ultrasound in the Emergency Department
Kemi Babagbemi, MD
Dr Babagbemi is an assistant professor of radiology and assistant attending radiologist at New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
In today’s evolving health-care environment, emphasis must be placed on providing accurate, safe, cost-effective, and timely diagnosis to the wide range of patients that present to the ED. To meet this need, emergency medicine physicians and radiologists have universally embraced the use of ultrasound in this setting.
Ultrasound is less expensive than computed tomography (CT) and magnetic resonance imaging (MRI), and its portability allows for bedside application, enabling its use in the most critical patients. It does not require extended preparation (eg, oral contrast) or carry the risk for adverse reactions associated with intravenously administered contrast. Also, since ultrasound does not use ionizing radiation, it is a particularly appropriate imaging option in susceptible populations such as pregnant and pediatric patients.1 Although a noninvasive modality, it can also be used to guide interventional procedures, including vascular access, thoracentesis/paracentesis, and specialized anesthesia.
Emergency physicians routinely perform ultrasound at bedside and are familiar with its utility in evaluating abdominal trauma, right upper quadrant pain, and acute biliary abnormalities; assessing vascular thrombosis or injury; and determining the etiology of pelvic pain and bleeding in both pregnant and nonpregnant patients. However, ultrasound is also increasingly being utilized to
diagnose other conditions for which CT and MRI were once thought the superior diagnostic tool.
Trauma (The Extended FAST Scan)
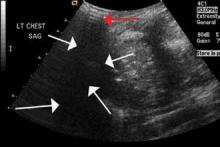
The focused abdominal sonography for trauma (FAST) scan has been used for rapid and immediate assessment of unstable trauma patients with suspected abdominal injury. In a recent study of 4,029 patients with blunt abdominal trauma, FAST scans had a sensitivity, specificity, and accuracy for detection of hemorrhage in patients with hypotension of 85%, 60%, and 77%, respectively.2 Other studies suggest that sonography of the chest may be useful in the rapid detection of additional life-threatening pathology such as pneumothorax (Figure 1), with data suggesting improved sensitivity over radiography.3 The inclusion of the pleural space in evaluation is increasingly more common and is referred to as the extended FAST (EFAST).
Appendicitis
The most common cause of abdominal pain requiring surgical intervention is appendicitis.4 Although certain clinically based prediction scores (eg, Alvarado scores) may be used, imaging is considered far superior in accurately diagnosing the condition.5 In a meta-analysis of data from 26 ultrasound and CT studies (15 prospective, 11 retrospective), there was a pooled 88% sensitivity and 94% specificity for ultrasound compared with CT, which exhibited a pooled sensitivity of 94% and specificity of 95%.6 As previously noted, because there is no ionizing radiation in ultrasound, it should be the preferred modality in both children and first-trimester pregnant patients.
Musculoskeletal Trauma
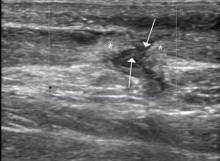
Ultrasound is an ideal imaging modality to evaluate the musculoskeletal system. Despite its widespread use in Europe for many years, musculoskeletal sonography is only now beginning to be adopted in the United States. Its ability to visualize soft-tissue structures makes it effective in evaluating for muscle, tendon, or ligament injury, and can even do so dynamically with stress maneuvers (Figure 2). With respect to fractures, sonography has also proved effective in evaluating for cortical disruption. For example, a recent study demonstrated overall 92% sensitivity and 100% sensitivity for fractures with high potential for complication in radiographically occult scaphoid fractures.7
Conclusion
As a true point-of-care imaging modality, ultrasound has an established place in the practice of emergency medicine. Future improvements in technology, including the ability to obtain true three-dimensional volumetric data sets, will expand its role even further.