Posterior Tibial Nerve Block
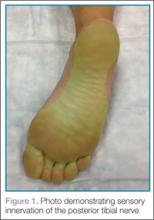
Emergency physicians (EPs) often treat injuries to the sole of the foot requiring laceration repairs or foreign body removal. Injecting local anesthetic directly into the sole of the foot is exquisitely painful given the lack of distensibility of the tissues and high concentration of nerve endings that are present. The posterior tibial nerve (PTN) provides sensory innervation to the majority of the sole of the foot (Figure 1). Given the superficial location of the nerve as well as its distal location, only small volumes of anesthetic are required and the risk of local anesthetic systemic toxicity is low, making the PTN block a great choice for the clinician new to nerve-block techniques. While the block is often performed using a blind approach, ultrasound guidance has been shown to improve success rates for this procedure1 and is easy to learn.Identifying the Posterior Tibial Nerve
To perform ultrasound of the PTN, the clinician should begin by palpating the posterior tibial artery just posterior to the medial malleolus. A high-frequency linear probe should then be placed over the artery (Figure 2). The PTN runs in a vascular bundle just posterior to the artery and can be identified by its hyperechoic, honeycomb appearance in the short axis (Figure 3). Sometimes sliding the probe up and down the leg a few centimeters can improve the ability to visualize the nerve.Performing the Block
To perform the block, a 22- to 25-gauge needle is advanced under the probe using an in-plane technique, so the entire shaft of the needle can be visualized as it approaches the nerve (Figure 4). The needle should typically enter the skin just anterior to the Achilles tendon. The needle is advanced until it almost touches the nerve, and 3 to 5 cc of local anesthetic is injected. If the patient experiences pain, the needle should be withdrawn to avoid direct intraneural injection and subsequent nerve injury. When the injection is successful, the clinician should see hypoechoic fluid circumferentially surround the nerve (An example of an ultrasound demonstrating this fluid distribution may be accessed at http://youtu.be/jR_VppydhlI).It is important to remember that the medial and lateral aspects of the sole of the foot receive variable degrees of innervation from the saphenous and sural nerves respectively; therefore, the EP should always ensure the area of interest is completely anesthetized before beginning the procedure.
Conclusion
Penetrating injuries to the sole of the foot are a common presentation in the ED. Achieving adequate anesthesia to the area with local anesthetic alone can be a difficult and painful process. However, with practice, ultrasound guidance can improve procedural success and decrease the risk of nerve injury as compared to blind nerve blocks.
Dr Beck is an assistant professor, department of emergency medicine, Emory University School of Medicine, Atlanta, Georgia. Dr Taylor is an assistant professor and director of postgraduate medical education, department of emergency medicine, Emory University School of Medicine, Atlanta, Georgia. Dr Meer is an assistant professor and director of emergency ultrasound, department of emergency medicine, Emory University School of Medicine, Atlanta, Georgia.