Case Reports
A Nervous Recipient of a “Tongue Lashing”
A veteran with a history of mental illness and drug and alcohol misuse developed a bleeding lesion on his tongue, which raised concerns of self-...
Reem Al Shabeeb is a Medical Student at the School of Medicine and Health Sciences at George Washington University. Caroline Trevisan is a Rheumatology Fellow and Amy Safadi is a Neurology Resident in the Departments of Internal Medicine and Neurology, both at MedStar Georgetown University Hospital, all in Washington, DC. Raj Singaraju is an Assistant Professor in the Department of Medicine at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
Correspondence: Raj Singaraju (raj.singaraju@usuhs.edu)
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
This patient was diagnosed with gastrointestinal beriberi. Because of her dietary changes, lactic acidosis, and bradycardia, thiamine deficiency was suspected after ruling out other possibilities on the differential diagnosis (Table). The patient’s symptoms resolved after administration of high-dose IV thiamine 500 mg 3 times daily for 4 days. Her white blood cell count and lactic acid level normalized. Unfortunately, thiamine levels were not obtained for the patient before treatment was initiated. After administration of IV thiamine, her plasma thiamine level was > 1,200 (normal range, 8-30) nmol/L.
Her differential diagnosis included infectious etiology. Given her leukocytosis and lactic acidosis, vancomycin and piperacillin/tazobactam were started on admission. One day later, her leukocytosis count doubled to 20.7×109 cells/L. However, after 48 hours of negative blood cultures, antibiotics were discontinued.
Small bowel obstruction was suspected due to the patient’s history of abdominal surgery but was ruled out with CT imaging. Similarly, pancreatitis was ruled out based on negative CT imaging and the patient’s normal lipase level. Gastroparesis also was considered because of the patient’s history of hypothyroidism, tobacco use, and her prior gastric-emptying study. The patient was treated for gastroparesis with a course of metoclopramide and erythromycin without improvement in symptoms. Additionally, gastroparesis would not explain the patient’s leukocytosis.
Cannabinoid hyperemesis syndrome (CHS) was suspected because the patient’s symptoms improved with cannabis discontinuation and hot showers.1 In chronic users, however, tetrahydrocannabinol levels have a half-life of 5 to 13 days.2 Although lactic acidosis and leukocytosis have been previously reported with cannabis use, it is unlikely that the patient would have such significant improvement within the first 4 days after discontinuation.1,3,4 Although the patient had many psychiatric comorbidities with previous hospitalizations describing concern for somatization disorder, her leukocytosis and elevated lactic acid levels were suggestive of an organic rather than a psychiatric etiology of her symptoms.
A veteran with a history of mental illness and drug and alcohol misuse developed a bleeding lesion on his tongue, which raised concerns of self-...
Further study of the long-term implications and follow-up is needed on SGLT2 mutation, an uncommon cause of glucosuria that mimics the effect of...
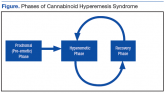
The convergence of legislative efforts, increasing prevalence, and tetrahydrocannabinol toxicity make this difficult-to-diagnose condition...
This uncommon delusion is associated with varied psychiatric, medical, iatrogenic, and neurologic conditions and may be difficult to fully resolve...
