Comorbidities and Medication Use
Hypertension (66%), hyperlipidemia (64%), and psychiatric diagnoses (50%) were most common comorbid conditions. Substance use (23%) and T2DM (40%) were the most common comorbidities influencing medication choice. Substance use evaluation included amphetamines and cocaine for this analysis.
Phentermine/topiramate is the preferred first-line agent unless patients have contraindications for use, in which case naltrexone/bupropion is recommended, based on guidelines for weight management medications within the VHI system. However, for patients with comorbid T2DM, liraglutide is preferred because of its beneficial effects for both weight loss and blood glucose control.2 Most patients at VHI were started on liraglutide (44%) or phentermine/topiramate (42%), which was in line with recommendations. Our sample included ≥ 1 prescription for each medication available at our facility, although the number of patients on each medication was not equal. Of note, the one patient taking lorcaserin at the time of study discontinued therapy in response to recent FDA guidance.9
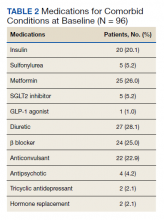
Medications for comorbid conditions could contribute to weight gain. Of the patient sample, β blockers (n = 24) and anticonvulsants, including gabapentin and pregabalin (n = 22) were the most common Other medications that could have contributed to weight gain included sulfonylureas (n = 5), antipsychotics (n = 4), tricyclic antidepressants (n = 2), and hormone replacement therapies (n = 2).
Primary Outcomes
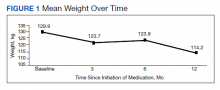
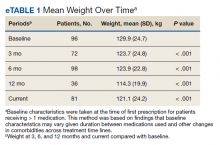
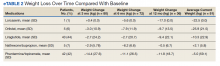
The mean weight of participants dropped from 129.9 to 114.2 kg over the 12 months of weight management medication therapy for a absolute difference of 15.8 kg (Figure 1 and eTable 1 available at doi:10.12788/fp.0117). Weight loss was recorded at 3, 6, 12, and > 12 months of weight management therapy. At each time point, weight loss was statistically significant (P < .001) compared with baseline (Table 2), even though not every patient had weight loss records at each time point.
When classified by medication choice, mean change in weight was orlistat −25.9 kg (n = 5); lorcaserin −22.5 kg (n = 1); liraglutide −10.3 kg (n = 43); phentermine/topiramate −5.0 kg (n = 42); and naltrexone/ bupropion +2.1 kg (n = 5) over the duration of the study (eTable 2 available at doi:10.12788/fp.0117). Patients receiving orlistat and liraglutide had increasing weight loss across the duration of treatment compared with those on lorcaserin who had initial weight gain before weight loss. Phentermine/topiramate showed initial weight loss that tapered off, and naltrexone/bupropion demonstrated initial weight loss with eventual weight gain at study end point.
Secondary Outcomes
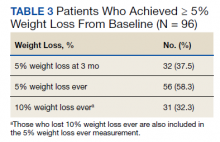
More than one-half of the patients analyzed lost 5 to 10% from baseline while taking weight management medication. Fifty-six (59%) patients lost 5% at any point while on therapy (Table 3). Among those patients, 31 (32%) lost ≥ 10% from baseline. When looking at success related to guideline recommendations, 32 (38%) patients lost 5% from baseline in the first 3 months of medication therapy.
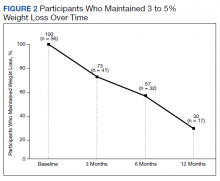
Among patients who lost at least 5% from baseline, we performed further analysis to assess weight maintenance of 3 to 5% from baseline for 12 months. In the 12 months after initial weight loss, the number of patients who were able to maintain their weight loss steadily declined (Figure 2). In the end, 17 (30%) of patients who achieved 5 to 10% weight loss at baseline were able to maintain weight loss. Only 18% of study patients were able to achieve guideline-directed weight loss and maintain that weight for 12 months.
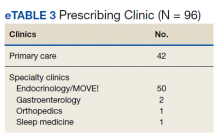
We found that most of our prescriptions (n = 50) were entered by the endocrinology department in conjunction with the MOVE! program (eTable 3 available at doi:10.12788/fp.0117). All 4 of our primary care clinics prescribed weight loss medication; however, 1 clinic prescribed the most. Other prescriptions came from community-based outpatient clinics or other specialties, including gastroenterology, orthopedics, and sleep medicine.
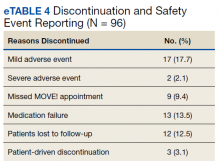
Nineteen (18%) patients experienced an adverse event (AE) that led to medication discontinuation, which was recorded in their chart (eTable 4 available at doi:10.12788/fp.0117). Most common AEs were GI upset with liraglutide or orlistat or dull aching and pain with phentermine/topiramate. Two severe AEs occurred: One patient experienced a change in mental health status and suicide attempt with naltrexone/bupropion; and 1 patient discontinued phentermine/topiramate because of a change in neurologic status.
Primarily medications were stopped because of inadequate weight loss (n = 13), and most patients tried additional medications. However, 1 medication failure resulted in sleeve gastrectomy. Other reasons for medication discontinuation included missed MOVE! appointments, patient lost to follow-up, and patient-elected discontinuation.