The first thing that comes to mind in this case is polyarteritis nodosa (PAN), an immune complex-mediated medium vessel disease that can involve large and small vessels in muscle, nerve, and skin. It can also present with masses.
►Dr. Apte: To address the arterial thrombi seen on CTA, arterial-brachial indices were obtained and showed bilateral occlusive disease in his distal extremities; findings that could be explained by vasculitis. His VATS biopsy pathology was reviewed for signs of vasculitis. Dr. Huang, can you review these slides for us please?
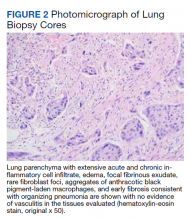
►Qin Huang, MD, Department of Pathology and Laboratory Medicine, VABHS and Assistant Professor of Pathology, HMS: This patient had a history of smoking, and there are many black pigment-laden macrophages present in the lung tissue. There were areas of hemorrhage and fibrin deposition and an overall picture of organizing pneumonia. At a lower power, you can see neutrophils everywhere, some in the form of micro-abscesses. The arterial walls did not show signs of vasculitis (Figure 2). Based on the clinical information and radiology findings, we suspected an acute infection-related pneumonia or a primary lung malignancy causing obstruction pneumonia. We suggested a rebiopsy of the lung mass to rule out a primary lung malignancy.
► Dr. Apte: Given his CT findings, a serologic rheumatologic workup including antineutrophil cytoplasmic antibody, antinuclear antibody, and rheumatoid factors were sent and returned negative. The location of arterial wall inflammation on imaging made it unamenable for biopsy. The patient began to experience bilateral temporal pain, which raised the concern for a large vessel vasculitis, specifically giant cell arteritis. Bilateral temporal artery biopsies were obtained and were not suggestive of vasculitis. Dr. Kaur, we still do not have any serologic or biopsy confirmation to support a diagnosis of vasculitis. Can we still call this a vasculitis?
►Dr. Kaur: Few things can cause the picture that was seen radiographically. A few noninflammatory causes like fibromuscular dysplasia can cause both large and small vessel stenosis, but the elevations in erythrocyte sedimentation rate and C-reactive protein along with response to steroids makes these diagnoses unlikely. Sometimes we must make a clinical diagnosis for vasculitis based on the clinical picture, and I would feel comfortable treating this patient for vasculitis.
With that said, I remain concerned that this patient also has a malignancy. His WBC increased to > 70 k/cm3 and his calcium to > 13 mg/dL. These findings are hard to explain by vasculitis alone. There are cancer-associated vasculitis, and I suspect this is the explanation here.8 His temporal pain was pointing to large vessel involvement, so he could have an undifferentiated vasculitis.
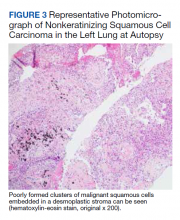
► Dr. Apte: A decision was made to empirically treat with tocilizumab, an IL-6 receptor antagonist, for an undifferentiated autoimmune disease, in addition to tapering steroids. The patient underwent a second VATS, which again revealed AFOP but no signs of malignancy. Unfortunately, he developed multiple complications over the subsequent weeks and passed away. An autopsy was requested by family members and pathology from his lung mass was reviewed. (Figure 3). Dr. Huang, can you review these slides for us?
► Dr. Huang: The left lung mass at autopsy shows nests, poorly formed clusters, and individuals of malignant neoplastic nonkeratinizing squamous cells embedded in a desmoplastic stroma in the mass center, consistent with poorly differentiated squamous cell carcinoma, and a circumscribed area of residual subacute organizing pneumonia with abscess, granulomatous changes, and early fibrosis at the periphery of this mass.
►Dr. Apte: Based on autopsy findings, the final diagnosis was poorly differentiated squamous cell carcinoma associated with subacute organizing pneumonia and medium vessel vasculitis, which presented with a severe leukocytosis ultimately thought to be a leukemoid reaction from his lung cancer.