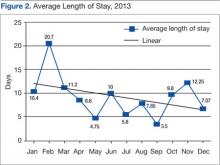
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
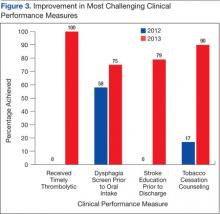
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.