A rise in medical malpractice insurance premiums and malpractice claims has brought the issue of medical malpractice to the forefront of medicine over the past few decades.1 The VA has more than tripled the number of legal settlements it has made over the past 5 years, and it has paid more than $871 million in medical malpractice settlements over the past decade.2,3 Legislation by the federal and state governments in the U.S., collectively referred to as tort reform, has been passed to curb the rate at which malpractice claims are filed; to set caps on noneconomic damages, such as pain and suffering; to control the effect of these claims on insurance premiums; and to prevent the delivery of negligent and harmful medical care.1
An observed high prevalence of medical malpractice claims has significant consequences within the clinical setting and has given rise to the practice of defensive medicine.4-8 Even the perceived threat of possible tort action may lead to aberrant practice behaviors. These defensive medical practices may include excessive testing, unnecessary referrals to other physicians or health facilities, or even refusal to treat particular patients.4,9-11 Furthermore, physicians devote valuable time and energy engaging in lawsuits rather than in delivering quality care to their patients.12
The increasingly litigious environment has discouraged physicians from practicing medicine, leading to earlier retirement, geographic relocation, and restriction of scope of services, all limiting patients’ access to health care.13 One such figure reported in 2008 found that in the U.S., defensive medicine costs can total nearly $56 billion.14 Radiation oncology is generally considered a medium-to-low risk specialty for litigation.15,16 Its average annual indemnity payment in 2006 was $276,792 and has increased at a rate of $1,500 per year, ranking it fifth among 22 specialty groups.16 Studies revealed that the practice of defensive medicine is not strictly limited to the U.S. and has been reported in other countries.6,17-20,21
A recent study by Jena and colleagues found that nearly 10% of oncologists face a malpractice claim annually, the 10th highest among the specialties surveyed.22 Malpractice within the field of radiation oncology has been previously discussed in the literature.16,23,24 There are limited data that examine the basis for these claims, the resulting jury verdicts, and the subsequent indemnity payments associated with claims.24,25
In this study, the authors sought to describe radiation oncology malpractice claims over the past 30 years. It is hoped that this study will not only help traditional oncologists in particular, but also all other practitioners who might be included as co-defendants to be more aware of the common causes of action that plaintiffs have been using to sue.
Methods
This public and online study did not involve human subjects research and accordingly did not require institutional review board approval. The WestlawNext (Thomson Reuters, New York) online legal database was used to search retrospectively for state and federal jury verdicts and settlements related to radiation oncology and medical malpractice. The database is a collection of several thousand search engines that can locate court dockets, jury verdicts, and settlements compiled by attorney-editors. Local cases and claims that were dismissed prior to proceeding to trial or that were settled out of court were not available. All cases in the database were considered and provided this study’s sample size, spanning from January 1, 1985, to December 31, 2015.
Given the boolean search functionality integrated into the Westlaw database, search parameters included “radiation oncology” and “medical malpractice” to yield the greatest number of cases (n = 223). All derived cases were manually reviewed, and files that were duplicates or associated with litigation unrelated to radiation oncology were excluded from analysis (n = 191).
Analysis
Factors that were collected and considered included the state and county in which the claim was filed, the age and sex of the litigant at the time of malpractice, the year the case was settled, co-defendant specialties, jury verdicts, award payouts, death status of the litigant and the alleged basis for the medical malpractice claim. A lack of informed consent, a failure to treat in a timely manner, a failure to order appropriate tests or to make a timely referral, misinterpretation of a test, excessive radiation, unnecessary radiation, unnecessary surgery, and procedural error all were included as alleged bases for the malpractice claim. Descriptive statistics were then compiled.
Results
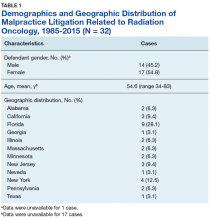
A total of 32 cases were included for analysis (Tables 1, 2, and 3). Anonymized summaries of all 32 cases are provided in the Appendix. The average age of the patient was 54.6 years (range 34-83) and included 17 (54.8%) female and 14 (45.2%) male patients.
The cases were distributed across 12 states, with 9 cases (28.1%) in Florida, 4 (12.5%) in New York, and 3 (9.4%) in California. Of 31 cases with available data, 19 suits (61.3%) were brought against 1 or 2 defendants, and 12 (38.7%) had ≥ 3 defendants. Radiation oncologists were defendants in all the cases. Otolaryngologists and orthopedic surgeons were the 2 most commonly named co-defendants, each named in 9.4% of cases.