The enzyme ADAR1 may be a therapeutic target for multiple myeloma (MM), according to research published in Nature Communications.
Investigators found that high ADAR1 levels correlate with reduced survival rates in MM patients.
The team also discovered that blocking ADAR1 reduced regeneration of high-risk MM in serially transplantable patient-derived xenografts.
The investigators believe that JAK2 inhibitors could be used to dampen ADAR1 activity and ultimately prevent progression or relapse in patients with MM.
“Despite new therapies, it’s virtually inevitable that a patient with multiple myeloma will experience relapse of the disease at some point,” said study author Catriona Jamieson, MD, PhD, of University of California, San Diego, in La Jolla.
“That’s why it’s exciting that this discovery may allow us to detect the disease earlier and address the root cause.”
Dr Jamieson and her colleagues knew that ADAR1 is normally expressed during fetal development to help blood cells form. The enzyme edits the sequence of RNA and is known to promote cancer progression and resistance to therapy.
With previous work, Dr Jamieson’s team described ADAR1’s contributions to chronic myeloid leukemia (CML). The enzyme’s RNA-editing activity boosts leukemic stem cells, giving rise to CML, increasing disease recurrence, and allowing CML to resist treatment.
For their current study, Dr Jamieson and her colleagues investigated ADAR1’s role in MM, first analyzing a database of nearly 800 MM patient samples.
The investigators found that patients with low ADAR1 levels in their tumor cells survived longer than patients with high ADAR1 levels.
While more than 90% of patients with low ADAR1 levels survived longer than 2 years after their initial diagnosis, fewer than 70% of patients with high ADAR1 levels did the same.
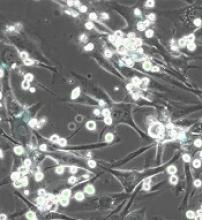
The investigators also created a humanized mouse model of MM and found that silencing the ADAR1 gene reduced the engraftment of MM.
“This is a difficult disease to model in animals; there isn’t a single gene we can manipulate to mimic multiple myeloma,” said study author Leslie A. Crews, PhD, of University of California, San Diego.
“This study is important, in part because we now have a new xenograft model that will, for the first time, allow us to apply new biomarkers to better predict disease progression and test new therapeutics.”
To advance their findings from this study, the investigators are exploring ways to leverage ADAR1 to detect MM progression as early as possible.
They are also testing inhibitors of JAK2, a molecule that influences ADAR1 activity, for their ability to eliminate cancer stem cells in MM models.
“Several major advances in recent years have been good news for multiple myeloma patients, but those new drugs only target terminally differentiated cancer cells and, thus, can only reduce the bulk of the tumor,” Dr Jamieson said.
“They don’t get to the root cause of disease development, progression, and relapse—cancer stem cells—the way inhibiting ADAR1 does. I like to call our approach ‘precision regenerative medicine.’”