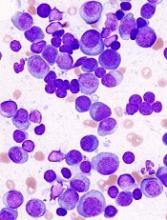
A cell-measuring technique can help predict how multiple myeloma (MM) patients will respond to different therapies, according to research published in Nature Communications.
The technique involves a microfluidic device known as a serial suspended microchannel resonator (sSMR).
The sSMR measures cell mass and allows researchers to calculate growth rates of single cells over short periods of time.
The device consists of a series of sensors that weigh cells as they flow through tiny channels.
The sSMR can measure 50 to 100 cells per hour.
Over a 20-minute period, each cell is weighed 10 times. This is enough to get an accurate mass accumulation rate (MAR), which is a measurement of the rate at which the cells gain mass.
With previous work, researchers showed that MAR can reveal drug susceptibility. A decrease in MAR following drug treatment means cells are sensitive to the drug. If cells are resistant, there is no change in MAR.
For the current study, Scott Manalis, PhD, of the Massachusetts Institute of Technology in Cambridge, and his colleagues tested drugs on cells from MM patients.
The team compared MAR results obtained via sSMR to outcomes of treatment in 9 patients.
For each patient, the researchers tracked the cells’ response to 3 different drugs—bortezomib, lenalidomide, and dexamethasone—plus combinations of those drugs.
In all 9 cases, the sSMR results matched the outcomes seen in patients, as measured by clinical biomarkers in the bloodstream.
“When the clinical biomarkers showed that the patients should be sensitive to a drug, we also saw sensitivity by our measurement,” said study author Mark Stevens, PhD, of the Massachusetts Institute of Technology and Dana-Farber Cancer Institute.
“[I]n cases where the patients were resistant, we saw that in the clinical biomarkers as well as our measurement.”
The researchers believe their device could potentially be used in MM patients at the time of relapse when the disease may have developed resistance to specific therapies.
“At this time of relapse, we would take a bone marrow biopsy from a patient, and we would test each therapy individually or in combinations that are typically used in the clinic,” Dr Stevens said. “At that point, we’d be able to inform the clinician as to which therapy or combinations of therapies this patient seems to be most sensitive or most resistant to.”
Now, the researchers are planning to conduct a larger clinical study to validate this approach. They also aim to investigate the possibility of using this technology for other cancers.
Some of the researchers involved in this study are cofounders of Travera and Affinity Biosensors, 2 companies that develop techniques relevant to this research.