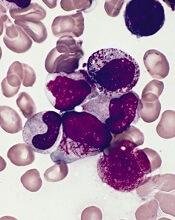
New research has revealed a way in which acute promyelocytic leukemia (APL) cells evade destruction by the immune system.
The study showed how group 2 innate lymphoid cells (ILC2s) are recruited by leukemic cells to suppress an essential anticancer immune response.
Researchers believe this newly discovered immunosuppressive axis likely holds sway in other cancers, and it might be disrupted by therapies already in use to treat other diseases.
Camilla Jandus, MD, PhD, of the Ludwig Institute for Cancer Research in Lausanne, Switzerland, and her colleagues described this research in Nature Communications.
“ILCs are not very abundant in the body, but, when activated, they secrete large amounts of immune factors,” Dr Jandus said. “In this way, they can dictate whether a response will be pro-inflammatory or anti-inflammatory.”
ILC1, 2, and 3 have been shown to play a role in inflammation and autoimmune diseases. However, their role in cancer has remained unclear.
To address that question, Dr Jandus and her colleagues began with the observation that one subtype of the cells, ILC2s, are abnormally abundant and hyperactivated in patients with APL.
The researchers examined ILC2 immunology in patients with active APL and compared it to that of APL patients in remission.
“Our analyses suggest that, in patients with this leukemia, ILC2s are at the beginning of a novel immunosuppressive axis, one that is likely to be active in other types of cancer as well,” Dr Jandus said.
She and her colleagues found that APL cells secrete large quantities of PGD2 and express high levels of B7H6 on their surface. Both of these molecules bind to receptors on ILC2s—CRTH2 and NKp30, respectively—activating the ILC2s and prompting them to secrete interleukin-13 (IL-13).
The IL-13 switches on and expands the population of monocytic myeloid-derived immune cells (M-MDSCs). These cells suppress immune responses and allow leukemic cells to evade immune system attack.
The researchers tested these findings in a mouse model of APL. Like patients, mice with APL displayed abnormal activation of ILC2s and M-MDSCs.
However, interfering with all the signals of the immunosuppressive axis restored anti-cancer immunity and prolonged survival in the mice.
Treating mice with a PGD2 inhibitor, an NKp30-blocking antibody, and an anti-IL-13 antibody resulted in reduced APL cell engraftment and a decrease in PGD2, ILC2s, and M-MDSCs. These mice also had significantly longer survival than untreated control mice (P<0.05).
Dr Jandus and her colleagues noted that antibodies against IL-13 and inhibitors of PGD2 are already in clinical use for other diseases, and antibodies that interfere with NKp30-B7H6 binding are in clinical development.
“We also found that this immunosuppressive axis may be operating in other types of cancer; in particular, prostate cancer,” Dr Jandus said. “We believe that some ILCs, like ILC2s, might suppress immune responses, while others might stimulate them. That’s what we are investigating in other types of tumors now.”
This research was supported by the Novartis Foundation for Medical-Biological Research, Ludwig Cancer Research, the Swiss National Science Foundation, Fondazione San Salvatore, ProFemmes UNIL, Fondation Pierre Mercier pour la Science, the Swiss Cancer League, and the Foundation for the Fight against Cancer.