The antibiotic tigecycline may enhance the treatment of chronic myeloid leukemia (CML), according to research published in Nature Medicine.
Using cells isolated from CML patients, researchers showed that treatment with tigecycline, an antibiotic used to treat bacterial infection, is effective in killing CML stem cells when used in combination with the tyrosine kinase inhibitor (TKI) imatinib.
The study also suggested the combination can stave off relapse in animal models of CML.
“We were very excited to find that, when we treated CML cells with both the antibiotic tigecycline and the TKI drug imatinib, CML stem cells were selectively killed,” said study author Vignir Helgason, PhD, of the University of Glasgow in Scotland.
“We believe that our findings provide a strong basis for testing this novel therapeutic strategy in clinical trials in order to eliminate CML stem cells and provide cure for CML patients.”
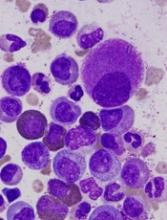
The researchers said they found that, in primitive CML stem and progenitor cells, mitochondrial oxidative metabolism is crucial for the production of energy and anabolic precursors. This suggested that restraining mitochondrial functions might have a therapeutic benefit in CML.
The team knew that, in addition to inhibiting bacterial protein synthesis, tigecycline inhibits the synthesis of mitochondrion-encoded proteins, which are required for the oxidative phosphorylation machinery.
So the researchers tested tigecycline, alone or in combination with imatinib, in CML cells. Both treatments (tigecycline monotherapy and the combination) “strongly impaired” the proliferation of primary CD34+ CML cells.
However, imatinib alone had “a moderate effect.” The researchers said this is in line with the preferential effect of imatinib on differentiated CD34− cells.
Each drug alone decreased the number of short-term CML colony-forming cells (CFCs), and the combination eliminated colony formation entirely. This correlated with an increase in cell death.
Neither monotherapy nor the combination had a significant effect on non-leukemic CFCs.
The researchers then turned to a xenotransplantation model of human CML. Starting 6 weeks after transplant, mice received daily doses of vehicle, tigecycline (escalating doses of 25–100 mg per kg body weight), imatinib (100 mg per kg body weight), or both drugs. All treatment was given for 4 weeks.
The team said there were no signs of toxicity in any of the mice.
Compared to controls, tigecycline-treated mice had a marginal decrease in the total number of CML-derived CD45+ cells in the bone marrow, and imatinib-treated mice had a significant decrease in these cells. But the CML burden decreased even further with combination treatment.
The researchers noted that imatinib alone marginally decreased the number of CD45+CD34+CD38− CML cells, but combination treatment eliminated 95% of these cells.
Finally, the team tested each drug alone and in combination (as well as vehicle control) in additional cohorts of mice with CML. After receiving treatment for 4 weeks, mice were left untreated for either 2 weeks or 3 weeks.
Mice that received imatinib alone showed signs of relapse at 2 and 3 weeks, as they had similar numbers of leukemic cells as vehicle-treated mice. However, most of the mice treated with the combination had low numbers of leukemic stem cells in the bone marrow.
“Our work in this study demonstrates, for the first time, that CML stem cells are metabolically distinct from normal blood stem cells, and this, in turn, provides opportunities to selectively target them,” said study author Eyal Gottlieb, PhD, of the Cancer Research UK Beatson Institute in Glasgow.
“It’s exciting to see that using an antibiotic alongside an existing treatment could be a way to keep this type of leukemia at bay and potentially even cure it,” added Karen Vousden, PhD, Cancer Research UK’s chief scientist.
“If this approach is shown to be safe and effective in humans too, it could offer a new option for patients who, at the moment, face long-term treatment with the possibility of relapse.”
This research was funded by AstraZeneca, Cancer Research UK, The Medical Research Council, Scottish Government Chief Scientist Office, The Howat Foundation, Friends of the Paul O’Gorman Leukaemia Research Centre, Bloodwise, The Kay Kendall Leukaemia Fund, Lady Tata International Award, and Leuka.