Researchers report that infusions of bone marrow-derived mesenchymal stromal cells (BM-MSCs) may be a treatment option for patients with aplastic anemia (AA) who are refractory to immunosuppressive therapy (IST).
They conducted a phase 2, non-comparative multicenter study to assess the safety and efficacy of this approach and found that after 12 months, 28.4% of patients responded, with 6.8% achieving a complete response (CR) and 21.6% a partial response (PR).
The trial involved 74 patients at 7 centers in China. The research team reported its findings in Stem Cells Translational Medicine.
About 30% to 40% of patients with severe AA (sAA) don’t respond well to IST and continue to have abnormally low levels of red blood cells, white blood cells, and platelets.
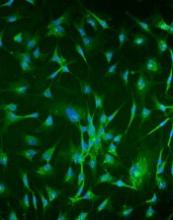
The benefit of treatment with BM-MSCs is they support hematopoiesis, express low levels of major histocompatibility (MHC)-I, and lack expression of MHC-II surface molecules.
And BM-MSCs have been reported to cure diseases, including graft-versus-host disease, arthritis, lupus, and other immune and non-immune disorders.
The current study, led by Yan Pang, MD, and Yang Xiao, MD, PhD, of Guangzhou General Hospital of Guangzhou Military Command in China, is based on their previous data evaluating intravenous administration of MSCs from a related donor in 18 patients with refractory AA.
This earlier data showed that 33% of patients with AA refractory to IST achieved a CR or PR to BM-MSC treatment.
So the team undertook to further investigate the use of BM-MSCs in AA.
Study design
Each of the 74 patients received 4 doses of BM-MSCs over a period of 4 weeks. If patients responded after the first month, they continued to receive 4 doses.
Investigators obtained the BM-MSCs from 74 healthy donors—48 males and 26 females. Forty were related donors, 27 haploidentical donors, and 7 unrelated donors.
Patients with AA by standard criteria had to be 16 years or older, had an incomplete response to antithymocyte globulin (ATG) and cyclosporine for at leas 6 months or cyclosporine alone for at least 12 months, did not have a donor available for bone marrow transplantation, and had at least one of the following: hemoglobin <70 g/L, neutrophilic granulocytes <1 × 109/L, or platelet count <30 × 109/L.
Almost half the patients (47%) were between 20 and 40 years, 54% were male, and 32% had severe aplastic anemia.
Patients’ previous therapy for aplastic anemia included cyclosporine and andriol (65%) cyclosporine and ATG (19%), and cyclosporine (16%).
Patients could continue cyclosporine, but no immunosuppressive agents were permitted.
Fifty-three patients (71.6%) completed 1 course of therapy, and 21 patients (18.4%) completed 2 courses.
Response
At 1 year, the overall response rate was 28.4% (n=21) and the PR rate was 21.6% (n=16).
The median time to a leukocyte response was 19 days (range, 11 – 29), to an erythrocyte response 17 days (range, 12 – 25), and to a megakaryocyte response 31 days (range, 26 – 84).
Ten of the patients with hematologic response had normalization of cellularity for more than 1 year.
The median follow-up among survivors was 17 months (range, 3 – 24). The 2-year overall survival was 87.8%.
Three patients progressed to myelodysplasia, 1 with refractory anemia with excess blasts (RAEB)-I and 2 with RAEB-II.
The median time to progression was 11 months (range, 8 – 12).
Nine patients died, all of whom had severe AA. One patient with RAEB-II died of disease progression, two patients died of intracranial hemorrhage, and six patients died of serious infection.
Safety
Adverse events included grade 1 (n=5) and grade 2 (n=2) fever. Two of these patients also had grade 1 headache.
The investigators observed no other adverse events.
Response predictors
The investigators determined that 2 factors predicted response in patients: prior treatment with antithymocyte globulin (ATG) and absence of infection throughout the treatment.
The odds ratio for patients treated with ATG was 1.41 (95% CI: -0.50, 3.31) and for patients without infection, 2.19 (95% CI: 0.50, 3.87).
“Our study strongly indicates that MSC infusion is a promising therapy for severe AA," Dr Pang said, “but improved MSC cultures in vitro and the MSC doses need further study to maximize their therapeutic potential."