VALENCIA, SPAIN—Phase 2 results suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with myelodysplastic syndromes (MDS).
Erythroid response rates were similar whether or not patients had received prior treatment with erythropoiesis-stimulating agents (ESAs).
However, patients without prior ESA exposure were more likely to achieve transfusion independence.
Most adverse events (AEs) considered possibly or probably related to luspatercept were grade 1 or 2.
Uwe Platzbecker, MD, of Universitätsklinikum Carl Gustav Carus in Dresden, Germany, presented these results at the 14th International Symposium on MDS.
The research was sponsored by Acceleron Pharma Inc., the company developing luspatercept in collaboration with Celgene Corporation.
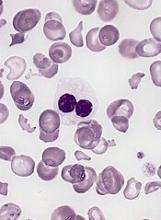
Dr Platzbecker explained that luspatercept, formerly ACE-536, is a modified activin receptor type IIB fusion protein that acts as a ligand trap for GDF11 and other TGF-βfamily ligands to suppress Smad2/3 signaling.
He presented data from a phase 2 base study and an extension study of luspatercept. The base study included 89 patients who received luspatercept for 3 months. The long-term extension study included 52 patients who may receive luspatercept for an additional 5 years.
The patients received luspatercept at doses ranging from 0.125 mg/kg to 1.75 mg/kg in the base study and 1.0 mg/kg to 1.75 mg/kg in the extension study. They received the drug subcutaneously every 3 weeks.
There were 82 patients evaluable for efficacy. They were a median of 2.3 years from diagnosis (range, 0-14). Their median age was 72 (range, 29-90), 63% were male, and 52% had prior treatment with ESAs.
The outcome measures used in these studies were clinically meaningful erythroid hematologic improvement per the International Working Group’s criteria (IWG HI-E) and red blood cell transfusion independence (RBC-TI).
IWG HI-E was defined as hemoglobin increase ≥ 1.5 g/dL sustained for ≥ 8 weeks in patients with a transfusion burden at baseline of less than 4 RBC units every 8 weeks and baseline hemoglobin levels below 10 g/dL. For patients with a greater transfusion burden at baseline, erythroid response was defined as a reduction of ≥ 4 RBC units sustained for ≥ 8 weeks.
RBC-TI was defined as no RBC transfusions for ≥ 8 weeks in patients with a baseline transfusion burden of at least 2 RBC units every 8 weeks.
Response data
In ESA-naïve patients, 48% (11/23) achieved RBC-TI with luspatercept, and 51% (20/39) achieved an IWG HI-E response.
Among patients with prior ESA treatment, 33% (11/33) achieved RBC-TI with luspatercept, and 51% (22/43) achieved an IWG HI-E response.
In patients with baseline erythropoietin (EPO) levels ≤ 500 international units per liter (IU/L), RBC-TI and IWG HI-E response rates were positive in both ring sideroblast-positive (RS+) and RS-negative (RS-) patients, according to the researchers.
| Baseline
EPO (IU/L) |
RS status | IWG HI-E, n=82
n (%) |
RBC-TI, n=56
n (%) |
| ≤ 500 | RS+ | 30/46 (65%) | 16/29 (55%) |
| RS- | 6/14 (43%) | 4/7 (57%) | |
| > 500 | RS+ | 5/9 (56%) | 2/9 (22%) |
| RS- | 1/11 (9%) | 0/9 (0%) | |
| Unknown | 0/2 (0%) | 0/2 (0%) |
*Table includes ESA-refractory and ESA-naïve patients. Patients treated at dose levels ≥ 0.75 mg/kg.
Safety data
All 89 patients were evaluable for safety. Common AEs (occurring in at least 3 patients) that were considered possibly or probably related to study drug were fatigue (6.7%), headache (6.7%), hypertension (5.6%), diarrhea (4.5%), arthralgia (3.4%), bone pain (3.4%), injection site erythema (3.4%), myalgia (3.4%), and peripheral edema (3.4%).
Grade 3 AEs possibly or probably related to study drug were ascites, blast cell count increase, blood bilirubin increase, hypertension, platelet count increase, and pleural effusion.
Grade 3 serious AEs possibly or probably related to study drug were general physical health deterioration and myalgia.