Blinatumomab has demonstrated activity in high-risk patients with Philadelphia chromosome-positive (Ph+) B-cell precursor acute lymphoblastic leukemia (BCP-ALL), according to research published in the Journal of Clinical Oncology.
This phase 2 trial enrolled patients with relapsed or refractory Ph+ BCP-ALL who had failed treatment with at least 1 tyrosine kinase inhibitor (TKI).
Blinatumomab produced a complete response (CR) in 31% of these patients, the median relapse-free survival was 6.7 months, and the median overall survival was 7.1 months.
The most common adverse events (AEs) were pyrexia, neurologic events, febrile neutropenia, and headache.
“Patients with Ph+ relapsed or refractory B-cell precursor ALL typically have lower remission rates, poor long-term prognosis, and shorter duration of remission than patients with Philadelphia chromosome-negative disease, and are especially in need of new treatment options beyond TKIs,” said study author Anthony Stein, MD, of City of Hope in Duarte, California.
“Results from this phase 2 study showed blinatumomab induced complete remission in these high-risk patients, regardless of prior TKI therapy or mutational status . . . .”
This study was supported by Amgen, the company developing and marketing blinatumomab.
The trial enrolled 45 patients with relapsed or refractory Ph+ BCP-ALL. Fifty-nine percent of patients had additional cytogenetic abnormalities. Forty-six percent had ABL1 kinase domain mutations, and 27% had the T315I mutation.
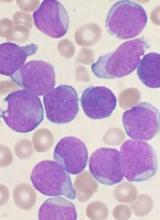
The patients’ median age was 55 (range, 23-78), and 55% were male. The median baseline bone marrow blast percentage was 80% (range, 6% to 98%).
Eighty-four percent of patients had received at least 2 prior TKIs. All patients were refractory to (56%), had relapsed on (33%), or progressed after (11%) TKI therapy. Forty-four percent of patients had undergone an allogeneic hematopoietic stem cell transplant (allo-HSCT).
The patients received blinatumomab in 28-day cycles by continuous intravenous infusion. The median number of cycles received was 2 (range, 1-5).
Efficacy
Thirty-six percent of patients (n=16) had a CR or CR with partial hematologic recovery (CRh) during the first 2 cycles of treatment. For 31% of patients (n=14), their best response was a CR.
Eighty-eight percent of patients who achieved a CR/CRh (n=14) achieved minimal residual disease (MRD) negativity.
Forty percent of patients with a T315I mutation had a CR/CRh (4/10), and all of these responders were MRD negative.
Seven responders (44%) went on to allo-HSCT, 6 of whom were transplant-naïve.
Eight of the 16 responders (50%) ultimately relapsed. Their median time to relapse was 6.7 months. Three patients relapsed during treatment, 2 relapsed without undergoing allo-HSCT, and 3 relapsed after allo-HSCT.
Seven responders (44%) were still alive and had not relapsed at last follow-up. The remaining responder died in CR after allo-HSCT.
The median relapse-free survival was 6.7 months, with or without censoring for allo-HSCT. And the median overall survival was 7.1 months, with or without censoring for allo-HSCT.
Safety
The most common AEs were pyrexia (58%), febrile neutropenia (40%), and headache (31%). Nearly half of patients (47%) had neurologic events.
Eighty-two percent of patients had grade 3 or higher treatment-emergent AEs. The most common were febrile neutropenia (27%), thrombocytopenia (22%), and anemia (16%).
Forty-four percent of patients had grade 3 or higher AEs that were considered possibly related to blinatumomab. The most common were febrile neutropenia and increased levels of alanine aminotransferase (11% each).
Five patients had fatal AEs—multiorgan failure, sepsis, septic shock, cerebral hemorrhage, and respiratory failure. The case of septic shock was considered related to treatment with blinatumomab.
Three patients developed cytokine release syndrome (all grade 1 or 2), but none of them had their treatment interrupted or discontinued as a result.
Three patients had grade 3 neurologic events, and 1 of these events (aphasia) required temporary treatment interruption. There were no grade 4 or 5 neurologic events.