The PI3K delta inhibitor idelalisib could turn chronic lymphocytic leukemia (CLL) into a highly treatable disease, according to the lead investigator of a phase 3 trial.
Results of the trial showed that adding idelalisib to treatment with rituximab can improve response and survival rates in patients with relapsed CLL.
In fact, the study was stopped early because idelalisib had a significant impact on progression-free survival.
“This study, and others we have conducted on idelalisib, demonstrates that we may no longer need to use chemotherapy in CLL,” said lead investigator Richard R. Furman, MD, of Weill Cornell Medical College in New York.
“Even if this cancer remains incurable, it now can be treated as if it was a chronic disease—with a pill, in the same way that high blood pressure is treated.”
Dr Furman and his colleagues reported the results of this study in The New England Journal of Medicine.
The trial was funded by Gilead, the makers of idelalisib. Dr Furman has served as an advisor for this company.
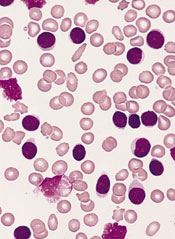
The study included 220 CLL patients who could not receive chemotherapy. Nearly two-thirds of the patients had advanced-stage disease. The median time from CLL diagnosis was 9 years, and patients had received a median of 3 previous treatments.
Most of the patients were 65 or older (78%). Forty percent had at least moderate renal dysfunction, and 35% had poor bone marrow function.
Half of the patients were randomized to receive idelalisib plus rituximab and the other half to rituximab plus placebo.
“It is remarkable how quickly idelalisib worked in this heavily treated group of patients, many of whom were resistant to chemotherapy,” Dr Furman said. “We saw responses within a week.”
Patients in the idelalisib arm had a much higher overall response rate than patients in the placebo arm—81% and 13%, respectively (P<0.001). But all responses were partial responses.
At 24 weeks, the rate of progression-free survival was 93% in the idelalisib arm and 46% in the placebo arm (P<0.001). The median progression-free survival was 5.5 months in the placebo arm and not reached in the idelalisib arm (P<0.001).
And at 12 months, the overall survival rate was 92% in the idelalisib arm and 80% in the placebo arm (P=0.02).
The difference in outcomes between the treatment groups prompted an independent data-monitoring committee to halt the study early, in October 2013, so that all participants could receive idelalisib.
Most adverse events (AEs), in either treatment group, were grade 2 or lower. The most common AEs in the idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the placebo arm, the most common AEs were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious AEs in the idelalisib arm than in the placebo arm—40% and 35%, respectively. The most frequent serious AEs were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Despite these events, the researchers considered idelalisib to be well-tolerated in this patient population.
“Having a treatment like idelalisib, which is highly effective and well-tolerated, and thus can generate responses in patients that are unable to tolerate treatment and unlikely to respond, indicates the potential for idelalisib in all patients,” Dr Furman said.

