A new strategy may one day prevent hemophilia patients from developing antibodies that inhibit clotting factors.
With this method, plant cells “teach” the immune system to tolerate the clotting factor protein.
In mice with hemophilia A, the strategy prevented and reversed the formation of factor VIII (FVIII) inhibitors.
Henry Daniell, PhD, of the University of Pennsylvania School of Dental Medicine in Philadelphia, and his colleagues described the approach in Blood. The work was supported by the National Institutes of Health and Bayer.
“The only current treatments for inhibitor formation cost $1 million and are risky for patients,” Dr Daniell said. “Our technique, which uses plant-based capsules, has the potential to be a cost-effective and safe alternative.”
Developing the technique
Previous studies had shown that exposing the immune system to individual components of the clotting factor protein could induce tolerance to the whole protein.
FVIII is composed of a heavy chain and a light chain, with each containing 3 domains. For their study, the researchers used the whole heavy chain and the C2 domain of the light chain.
Dr Daniell and his colleagues developed a platform for delivering drugs and biotherapeutics that relies on genetically modifying plants so they express the protein of interest.
Trying that same method with the components of the FVIII molecule, the team first fused the heavy chain DNA with DNA encoding a cholera toxin subunit, a protein that can cross the intestinal wall and enter the bloodstream, and did the same with the C2 DNA.
They introduced the fused genes into tobacco chloroplasts, so that some plants expressed the heavy chain and cholera toxin proteins and others expressed the C2 and cholera toxin proteins. They then ground up the plant leaves and suspended them in a solution, mixing the heavy chain and C2 solutions together.
Testing in mice
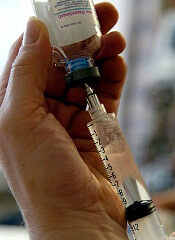
The researchers fed the mixed solution to mice with hemophilia A twice a week for 2 months and compared them to mice that consumed unmodified plant material. The team then gave the mice infusions of FVIII.
As expected, the control mice formed high levels of inhibitors. But the mice fed the experimental plant material formed much lower levels of inhibitors—on average, 7 times lower.
Mice that consumed the experimental plants exhibited upregulation of cytokines associated with suppressing or regulating immune responses, while control mice showed upregulation of cytokines associated with triggering an immune response.
By transferring subsets of regulatory T cells taken from the mice that received the experimental plants into normal mice, the researchers were able to suppress inhibitor formation. This suggests the T cells were able to carry tolerance-inducing characteristics to the new population of animals.
“This gives us an explanation for the mechanism of how this tolerance is being created,” Dr Daniell said.
Finally, the researchers tried to reverse inhibitor formation. They fed the experimental plant material to mice that had already developed inhibitors.
Compared to a control group, the mice given the FVIII-containing plant material had their inhibitor formation slow and then reverse, decreasing 3- to 7-fold over 2 or 3 months of feeding.
This strategy holds promise for preventing and even reversing inhibitor formation in hemophiliacs receiving FVIII infusions. However, the researchers’ experiments showed that inhibitor levels could rise again as time passes.
“After some time, antibodies do develop if you stop giving them the plant material,” Dr Daniell said. “This is not a one-time treatment. You need to do it repetitively to maintain the tolerance.”
Dr Daniell and the Penn Center for Innovation are now working with a pharmaceutical company to test this oral tolerance strategy in other animal species, with plans to begin human trials shortly thereafter. For human use, the goal would be to use lettuce plants instead of tobacco plants.

