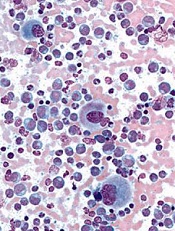
Credit: UC San Diego
In vitro experiments have revealed new insight into tyrosine kinase inhibitor (TKI) resistance among patients with chronic myeloid leukemia (CML).
Though it’s now possible to overcome TKI resistance resulting from single BCR-ABL1 mutants, targeting compound mutants remains a challenge.
So researchers tested several TKIs on various BCR-ABL1 compound mutants to determine which drug, if any, would be most effective for each combination.
The results appear in Cancer Cell.
Thomas O’Hare, PhD, of the Huntsman Cancer Institute at the University of Utah, and his colleagues first took an inventory of clinical BCR-ABL1 compound mutations associated with TKI resistance that had been reported in the literature.
The team identified 12 kinase domain positions that account for most clinical BCR-ABL1 TKI resistance—M244, G250, Q252, Y253, E255, V299, F311, T315, F317, M351, F359, and H396.
All of the clinically reported compound mutations include at least 1 of the 12 key positions, and most (65%) include 2. Each position has been implicated in resistance to 1 or more TKIs, including imatinib, nilotinib, dasatinib, bosutinib, rebastinib, and ponatinib.
The researchers found that some of the compound mutations they studied conferred resistance several-fold higher than that of either contributing mutation alone.
“We were able to sequence about 100 clinical samples, which gave us a very large body of data to shed light on the number of compound mutations and how they develop,” said Michael Deininger, MD, PhD, also of the Huntsman Cancer Institute.
“One key finding was that compound mutations containing an already known mutation called T315I tend to confer complete resistance to all available TKIs.”
The researchers had focused their testing on ponatinib, as the drug has proven effective against resistant CML, particularly cases with the T315I mutation. Unfortunately, ponatinib was often no match for compound mutations including T315I.
Tests did suggest that a 30 mg/day dose of ponatinib would maintain efficacy against 7 of the 8 non-T315I compound mutants tested, though the Y253H/E255V mutant proved resistant.
The researchers also found that a 15 mg/day dose of ponatinib could pre-empt outgrowth of 5 of the 8 non-T315I compound mutants, though Y253H/E255V, E255V/V299L, and F317L/F359V might be problematic.
But ponatinib proved substantially less effective against T315I-inclusive compound mutants. Nine of 10 T315I-inclusive compound mutants showed little or no sensitivity to ponatinib or any of the other TKIs tested. M244V/T315I was the only compound mutant not resistant to ponatinib.
The researchers noted that because ponatinib has proven effective against the T315I mutant in isolation, many patients treated with ponatinib are likely to have this mutation.
So it may be necessary to perform more sensitive screening on these patients to determine whether they might have T315I-inclusive compound mutants that could confer resistance.
“Fortunately, the problems we are studying affect a minority of CML patients,” Dr O’Hare said. “[S]till, this leaves some patients with no good treatment option at all. Our goal is to have a TKI option for every patient.”
According to Dr O’Hare, it’s only a matter of time until analogous compound mutations emerge in many other cancers, including acute myeloid leukemia and non-small cell lung cancer.
“Our findings in CML will provide a blueprint for contending with resistance in these highly aggressive diseases as well,” he concluded.

