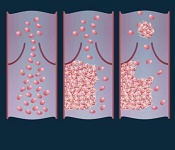
vein (left), thrombus formation
(middle), and a thrombus (right)
detaching from a vessel wall,
leading to thromboembolism.
Image by Moscow Institute
of Physics and Technology
Photoacoustic flow cytometry (PAFC) can provide real-time, non-invasive detection of emboli, according to research published in PLOS ONE.
Experiments in mice showed that PAFC can reveal emboli triggered by melanoma and medical procedures by detecting transient changes in blood absorption.
Investigators believe that by providing early embolus detection, PAFC could enable well-timed anticoagulant therapy and potentially prevent lethal complications.
For this study, the team used PAFC to monitor embolus formation in 4 groups of mice.
Two of the groups had melanoma. In one, the implanted tumor underwent compression. In the other, the investigators performed a surgical excision of the tumor.
The remaining 2 groups consisted of healthy mice. In one of these groups, mice had their limbs clamped to produce vessel stasis. In the other, the mice underwent surgery.
The investigators found that PAFC could detect a single embolus, and the method allowed them to distinguish between erythrocyte-rich and leukocyte/platelet-rich emboli.
They also observed a correlation between the presence of white emboli and melanoma.
The level of circulating emboli was significantly higher in the melanoma-bearing mice than in the healthy ones (P=0.0013).
However, the number of circulating emboli temporarily increased in the healthy mice during vessel stasis (P=0.033) and after surgical excisions (P=0.031).
The melanoma-bearing mice also experienced increases in the number of circulating emboli during tumor compression (P=0.013) and after tumor excision (P=0.012).
“We showed that it is possible to detect emboli in the bloodstream using photoacoustic flow cytometry,” said study author Alexander Melerzanov, PhD, of the Moscow Institute of Physics and Technology in Russia.
“PAFC may also be used to destroy blood clots, and we hope to work on this in our next experiments.”


