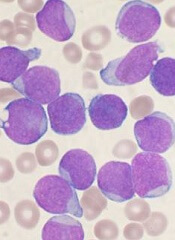
In tracing the clonal evolution of B-cell acute lymphoblastic leukemia (B-ALL) from diagnosis to relapse, researchers discovered that clonal diversity is comparable in both states.
They also identified mutations associated with B-ALL relapse and found that clonal survival is not dependent upon mutation burden.
In most of the cases the researchers analyzed, a single, minor clone survived therapy, acquired additional mutations, and drove disease relapse.
Jinghui Zhang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues recounted these findings in Nature Communications.
The researchers performed deep, whole-exome sequencing on cell samples from 20 young patients (ages 2 to 19) with relapsed B-ALL. The samples were collected at diagnosis, remission, and relapse.
“[W]e wanted to find out the underlying mechanism leading to cancer relapse,” Dr Zhang said. “When the cancer recurs, is it a completely different cancer, or is it an extension, or change, arising from pre-existing cancer?”
The researchers were able to detect the mutations in both the “rising” and “falling” clones—those that survive therapy and those that don’t—at the different disease stages and pinpoint the mutations that drove the leukemia.
Seven genes were highly likely to be mutated in relapsed disease—NT5C2, CREBBP, WHSC1, TP53, USH2A, NRAS, and IKZF1.
The researchers also characterized how diverse those mutations were at diagnosis and relapse. They found that B-ALL cells were mutating just as wildly and diversely in one phase of disease as in the other.
“This finding was interesting, because most people think that the clone that has the most mutations is more likely to survive therapy and evolve, but that doesn’t seem to be the case,” Dr Zhang said.
In most cases, relapse was driven by a minor subclone that had survived therapy and was present at an extremely low level. The researchers said this finding suggests a need to change the way we assess patients after treatment to determine the likelihood of relapse.
“When we are analyzing for the level of minimum residual disease in monitoring remission in patients, we should not only pay attention to the mutations in the predominant clone,” Dr Zhang said. “We should also be tracking what kinds of mutations exist in the minor subclones.”


