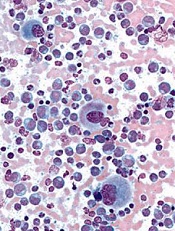
Image from UC San Diego
Scientists say they have developed a model that can be used to calculate the proportion of cancer stem cells (CSCs) present over the course of treatment.
The model is designed to enable estimation of CSC fractions from longitudinal measurements of tumor burden.
The scientists tested the model in patients with chronic myeloid leukemia (CML) and found evidence to suggest the proportion of CSCs increases
substantially during extended treatment.
The team believes the model could eventually be used to help doctors predict tumor development and help them select suitable treatments for cancer patients.
“Cancer stem cells not only promote the growth of a tumor, they can also be resistant to radiotherapy and chemotherapy,” said Philipp Altrock, PhD, of the Dana Farber Cancer Institute in Boston, Massachusetts.
“If we can estimate the number of cancer stem cells at diagnosis and over the course of treatment, the treatment can be tailored accordingly.”
Dr Altrock and his colleagues discussed this possibility in Cancer Research.
The team first explained that their model incorporates tumor dynamics and tumor burden information. They said tumor expansion and regression curves can be leveraged to estimate the proportion of CSCs in individual patients at baseline and during therapy.
To test their model, the scientists used 2 independent cohorts of CML patients. The team evaluated the growth and decline of CML over the course of treatment with the tyrosine kinase inhibitor imatinib.
Based on the change of disease burden during treatment, the model calculated the proportion of CSCs.
Results suggested the proportion of CSCs in CML patients increases 100-fold after a year of treatment with imatinib. And that proportion continues to increase up to 1000-fold after 5 years of treatment.
The scientists noted that this model is parameter-free, so it can be applied to different types of cancer. However, they said further development is required before the model can be used in clinical practice.


