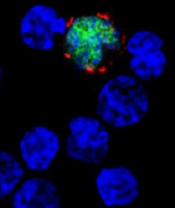
among uninfected cells (blue)
Image courtesy of NIH/
Benjamin Chaigne-Delalande
PHILADELPHIA—Cytotoxic T lymphocytes designed to target Epstein-Barr virus (EBV-CTLs) can elicit durable responses in patients
with EBV–associated lymphoproliferative disorder (EBV-LPD), according to data presented at the AACRAnnual Meeting 2015.
Results from two trials showed that EBV-CTLs derived from a patient’s transplant donor could produce a response rate of 62%, and EBV-CTLs derived from third-party donors could produce a response rate of 61%.
Study investigators noted that, with the achievement of complete response (CR), remission proved durable. And, unlike with chemotherapy, partial responses (PRs) to EBV-CTLs were durable as well.
The team presented these results as abstract CT107.*
“The purpose of our clinical trials was to see if giving T cells from a normal-immune individual that were expanded in culture and stimulated to respond to multiple proteins from the Epstein-Barr virus could provide a safe and effective treatment,” said Richard J. O’Reilly, MD, of Memorial Sloan Kettering Cancer Center in New York.
“The good news from our two clinical trials is that EBV-CTLs generated from either the patient’s transplant donor or from the bank of normal donor T cells developed at Memorial Sloan Kettering put aggressive EBV-LPD that had failed to respond to rituximab into long-lasting remission in more than 60% of patients.”
In the first trial, 26 patients with EBV-LPD received EBV-CTLs generated from their transplant donor. Thirteen of these patients had previously received rituximab, and 16 had high-risk disease.
Thirteen patients in this trial received HLA-matched, EBV-CTLs from the Memorial Sloan Kettering Cancer Center bank of EBV-CTLs generated from third-party, healthy donors. All 13 patients had high-risk disease, and 12 had received prior rituximab.
Dr O’Reilly noted that good results were observed with EBV-CTLs from both sources in this trial. And because EBV-CTLs from the bank are available immediately, he and his team used only EBV-CTLs from the bank when treating the 18 patients enrolled in the second trial.
Among the 39 patients enrolled in the first trial, 23 had a CR, none had a PR, and 2 had stable disease.
For patients who received EBV-CTLs from their primary donor, the combined rate of CR and PR was 62% (16 CRs). For patients who received third-party EBV-CTLs, the combined rate of CR and PR was 54% (7 CRs).
Sixteen of the patients who achieved a CR are still doing well, Dr O’Reilly said. Eight of these patients are alive more than 5 years after receiving EBV-CTLs, and 1 is alive more than 10 years after treatment.
Among the 18 patients enrolled in the second trial, 9 had a CR, 3 had a PR, and 1 had stable disease. The combined rate of CR and PR was 67%.
All of the patients who achieved a CR in this trial continue to do well, and the investigators will be following them long-term, Dr O’Reilly said.
He also noted that toxicities with EBV-CTLs were minimal, and there were no treatment-related deaths. None of the patients developed cytokine release syndrome or graft-vs-host disease requiring systemic therapy.
“The EBV-CTLs work well for the majority of recipients,” Dr O’Reilly said. “However, the responses became clinically evident only after the T cells expanded in vivo, which took about 7 to 14 days. We are rigorously pursuing the development of biomarkers or other tests to predict response earlier.”
Memorial Sloan Kettering Cancer Center has entered into an option agreement with Atara Biotherapeutics to further develop EBV-CTLs for clinical use. However, the data presented at AACR were accrued prior to that agreement.
Last month, the US Food and Drug Administration granted breakthrough therapy designation to EBV-CTLs generated from third-party donors for the treatment of patients with rituximab-refractory EBV-LPD.

*Information in the abstract differs from that presented at the meeting.

