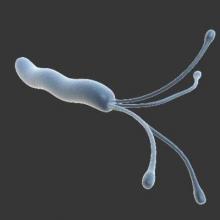
For the first time, an oral vaccine against Helicobacter pylori infection proved effective and safe in a phase III trial involving nearly 4,500 children in China, according to a report published in the Oct. 10 issue of the Lancet.
The vaccine’s efficacy waned somewhat after the first year but still significantly reduced H. pylori infection in approximately 1,000 of the recipients followed for the entire 3-year study period. This suggests that it could substantially reduce the rates of gastritis, peptic ulcer, gastric adenocarcinoma, and lymphoma associated with the infection, which currently affects more than half the world’s population, including more than 600 million in China, said Ming Zeng, Ph.D., of the Chinese National Institute for Food and Drug Control, Beijing, and associates.
Researchers at Third Military Medical University, Chongqing and Chongqing Kangwei Biotechnology, both in China, developed the new vaccine using DNA recombination technology to fuse urease B subunit proteins (gene derived from H. pylori) with heat-labile enterotoxin B subunit proteins (gene derived from E. coli). The vaccine was designed to be administered in three oral doses given 2 weeks apart, after study subjects fasted for at least 2 hours and then drank an 80-mL buffer solution containing sodium bicarbonate and sodium citrate.
Dr. Zeng and associates compared the vaccine (2,232 participants) against an identical placebo (2,232 participants) in the single-center, double-blind, randomized trial, which involved children aged 6-15 years recruited from 12 schools in Ganyu County in eastern China. All the study participants were healthy and tested negative for past or present H. pylori infection at baseline.
The primary endpoint – the development of H. pylori infection within the first year after vaccination – occurred in 14 children who received the vaccine, which was significantly fewer than the 50 children who received placebo. This yielded a vaccine efficacy rate of 71.8% at 1 year. During extended follow-up of a subset of 3,014 participants at 2 years, 10 H. pylori infections developed in the vaccine group and 22 in the placebo group, for a vaccine efficacy of 55.0%. Similarly, at 3-year follow-up of 1,946 participants, vaccine efficacy was 55.8%, the investigators said (Lancet 2015 Oct 10;386:1457-64).
“The event rate of the placebo group varied from 2.4 to 1.4 per 100 person-years, whereas that of the vaccine group remained around 0.7/100 person-years” throughout the 3-year study period, they added.
The vaccine elicited a significantly greater immune response than did the placebo, as measured in serum IgG and salivary IgA. The geometric mean titer was 389.4 in vaccine recipients, compared with only 72.2 in the placebo group, and the seroconversion rate was 86.1% for the vaccine, compared with 4.6% for placebo. The “mild” waning trend in vaccine-elicited antibodies suggests that a booster dose may be necessary in later years, Dr. Zeng and associates wrote.
The incidence of adverse reactions to the vaccine was identical in the two study groups, at 7%. All adverse reactions were mild and resolved within 24 hours. The most frequent was vomiting, followed by fever and headache. No serious adverse events were considered to be related to the study drug. “However, the number of participants in this study might not be enough to identify rare vaccine-related adverse events. Longer-term follow-up is needed in much larger populations” and in more ethnically and demographically diverse groups to identify such rare reactions, they noted.