AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
Ultrasound-detected crystal depositions decreased over the course of the 1-year study for all three ultrasound signs considered, researcher Hilde B. Hammer, PhD, reported at the European Congress of Rheumatology.“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
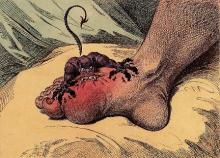
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.