PARIS – Bioabsorbable vascular scaffolds have caught on in Europe and elsewhere in the world as an alternative to conventional metal stents for percutaneous coronary interventions in a wide spectrum of patient types.
By May 2014, more than 50,000 bioabsorbable vascular scaffolds (BVS) of the first brand to enter the European market – the Absorb stent made by Abbott Vascular – had gone into patients since the first placement in 2007, with the vast majority placed since this scaffold entered the European market in September 2012. Use of BVS in the United States remains investigational, while in the 20-plus months since BVS first became available in Europe other brands of BVS also have entered that market.
Despite growing BVS use in Europe, as well as in Asia and Central and South America, where they are also available, large-scale data on the consequences, especially long-term consequences, of BVS placement are mostly lacking, particularly data on how BVS perform when directly compared with drug-eluting metallic stents.
"Today we have uncontrolled dissemination of the technology without comparative data," Dr. Patrick W. Serruys, a pioneer in using BVS, said during a session at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
"We need evidence to know exactly what to do" with BVS, which patients to use them in, and when they are preferable to metallic stents, said Dr. Serruys, an interventional cardiologist and professor of medicine at the Thoraxcenter of Erasmus University in Rotterdam, the Netherlands.
"In the 7 years I’ve used them, in patients with 5-year follow-up, there have been no negative signals," he said in an interview, discussing his part of the sizeable anecdotal experience that BVS are safe and effective.
Several large trials comparing BVS with metal stents are in progress, including U.S. pivotal trials, but until these results are out, all that interventionalists have to gauge BVS performance are results from registries and uncontrolled trials. Given that limitation, so far the data look uniformly excellent.
"It is clear that emerging data from real-world, expanded-use registries suggest that use of the Absorb BVS is feasible and safe in a variety of patients, from low to high risk, and from simple to complex lesions," said Dr. Gregg W. Stone in a talk at the meeting. "But attention to procedural detail and technique is essential to optimize the outcomes. BVS are a little more complicated than metallic drug-eluting stents," said Dr. Stone, professor and director of cardiovascular research and education at Columbia University in New York.
"Data from large, randomized controlled trials are necessary to demonstrate whether BVS truly improve outcomes compared with best-in-class metallic stents. We are still early in the technology," he said. Dr. Stone is a lead investigator for one of the large U.S. randomized trials comparing the Absorb BVS to the current standard for percutaneous coronary interventions, a second-generation drug-eluting metallic stent.
Hints of what BVS may deliver
Hints of some of the potential benefits that BVS might provide appeared in results from a post-hoc, across-studies analysis that Dr. Stone presented in his talk. He compared the incidence of angina during the first year following PCI in 287 patients from the Absorb EXTEND study and 602 patients who received coronary stenting with the Xience second-generation everolimus-eluting metallic stent in the SPIRIT IV trial. The analysis matched patients in the Absorb arm with those in the Xience arm by propensity scoring.
The 1-year angina rates were 28% for the patients who received a metallic stent and 16% for those who received an absorbable scaffold, a 12% absolute difference, with a hazard ratio showing a 47% relative reduction in angina in patients who received the BVS, Dr. Stone reported. "There are a variety of mechanisms" by which BVS might reduce the rate of angina compared with metallic stents, including restoration of cyclic pulsatility in the treated arteries and improved vasomotion, he said.
The two outstanding clinical issues that dog PCI with second-generation drug-eluting metallic stents are the accrual of "very late" adverse events and the slow return of angina, with an average rate of target lesion failure with second-generation stents of about 1.8% year that continues out for at least 5 years, he said. "Can BVS flatten out the ongoing event rate" and improve measures like recurrent angina? Dr. Stone asked.
In another cross-study comparison, Dr. Serruys cited a recent, still unpublished analysis on which he collaborated that compared the 1-year outcomes of 102 patients with diabetes who received a BVS and 172 patients with diabetes who received a second-generation drug-eluting metallic stent. The 12-month cumulative rate of cardiovascular death, myocardial infarction, or ischemia-driven target lesion revascularization was 34.9% in the BVS recipients and 6.4% in patients who received state-of-the-art drug-eluting stents.
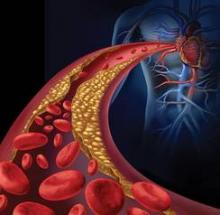
The working hypothesis behind BVS is that, by dissolving during a period of 12-24 months, the scaffold provides temporary bracing against restenosis but then disappears, allowing improved endovascular healing. During a separate session at EuroPCR, Dr. Charles A. Simonton, an interventional cardiologist and chief medical officer for Abbott Vascular, described the hypothesized impact that bioabsorbable coronary stents might have.
"Our vision is to convert interventional cardiology from mechanically oriented, plumbing-type interventions where you do mechanical things to open arteries" to a focus on tissue regeneration. "What we see when scaffolds resorb is that, at 3-5 years, the arteries look very different from what we see with a metal stent. The vessels show a highly functional neointimal layer that is functioning smooth muscle cells that protect against rupture in underlying plaque," he said.
Having BVS will allow interventional cardiologists to "transition from being mechanical plumbers to really being medical doctors. Not just opening lesions but putting in a treatment that can improve patients long term," Dr. Simonton said, presenting his best-case prediction of what BVS might achieve. "We need to generate a lot of data to make sure this is real," he added, in something of an understatement.
"There is late lumen enlargement with BVS. That is a clear fact," said Dr. Serruys.