Clinical Review
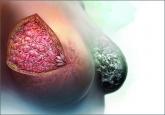
Atypical hyperplasia of the breast: Cancer risk-reduction strategies
Women with atypical hyperplasia are at increased risk for breast cancer. We need to characterize that risk for patients and ensure appropriate...
Laila Samiian, MD, and Andrew M. Kaunitz, MD
Dr. Samiian is Assistant Professor and Chief, Section of Breast Surgery, at the University of Florida College of Medicine–Jacksonville. Dr. Samiian serves as the Director of the University of Florida Health Jacksonville Multidisciplinary Breast Conference.
Dr. Kaunitz is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He is also Director of Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists–Emerson. He serves on the OBG Management Board of Editors.
The authors report no financial relationships relevant to this article.

Counsel precisely and accurately. Beyond such testing, we should focus on what is important to our patients in explaining the diagnosis:
Informed and shared
decision making is key
DCIS is an increasingly common and usually non–life-threatening condition. Radical surgery such as bilateral mastectomy for small unifocal DCIS is excessive and will not improve a patient’s outcome. As a prominent breast surgeon has written:
We must balance the small risk of breast cancer recurrence after lumpectomy for DCIS with patients’ quality of life concerns. This goal is best accomplished by using an informed and shared decision-making strategy to help our patients make sound decisions regarding DCIS.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Women with atypical hyperplasia are at increased risk for breast cancer. We need to characterize that risk for patients and ensure appropriate...
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...
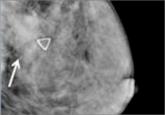
An expert radiologist and dense breast educators address specific questions that will arise in your counseling and care of women who are...

A single, medically sourced resource for you and your patients on dense breasts exists. It is called DenseBreast-info.org, and its founders...
