News for Your Practice

What you should know about the latest change in mammography screening guidelines
When the American Cancer Society issued new guidelines, key stakeholders responded with a “Yay” or “Nay”—and sometimes both. How should you...
Dr. Kopans is Professor of Radiology at Harvard Medical School and Senior Radiologist in the Breast Imaging Division at Massachusetts General Hospital in Boston, Massachusetts.
Dr. Kopans reports that he receives grant or research support from General Electric and is a consultant to General Electric and Hologic. Massachusetts General Hospital holds his patent on digital breast tomosynthesis.

Here are the proven facts about breast cancer screening
Why not screen only high-risk women? It has been suggested that only high-risk women should participate in screening. However, women who inherit a genetic predisposition account for only about 10% of breast cancers each year.39 If we add to that number other women with family histories or other known risk factors, these cases account for another 15% of cancers.40
Regrettably, high-risk women account for only a quarter of breast cancers diagnosed each year. If only high-risk women are screened, the vast majority of women who develop breast cancer (75%) will not benefit from early detection.
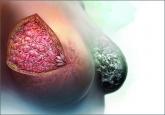
The bottom line Mammography is not perfect. It does not find all cancers and does not find all cancers early enough for a cure. However, there is no universal cure on the horizon, while screening is available today and is saving thousands of lives each year.
All women should have access to, and be encouraged to participate in, annual screening starting at age 40.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.

When the American Cancer Society issued new guidelines, key stakeholders responded with a “Yay” or “Nay”—and sometimes both. How should you...
Confused about which guidelines for breast cancer screening to follow in average-risk women? ACOG takes action with an upcoming consensus...
An expert radiologist and dense breast educators address specific questions that will arise in your counseling and care of women who are...
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...
