Fistula developed after delivery: $50M verdict
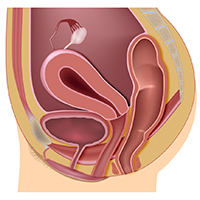
During delivery of a 31-year-old woman's baby, a nuchal cord was encountered. In order to safely deliver the child, the ObGyn performed an episiotomy.
After delivery, the patient reported an odorous vaginal discharge. The ObGyn explained that the condition was a natural byproduct of delivery and suggested that it would resolve without treatment.
The patient became pregnant a second time shortly after her first delivery and was evaluated by a midwife. The patient again reported the odorous discharge, but the condition was not addressed. At delivery of her second child, the ObGyn determined that the patient had a rectovaginal fistula. The patient underwent 13 repair operations.
PATIENT’S CLAIM:
The fistula was a byproduct of the episiotomy performed during the first delivery. The episiotomy should not have been performed. The ObGyn should have diagnosed and treated the fistula prior to delivery of the second child and performed a cesarean delivery.
DEFENDANT'S DEFENSE:
The ObGyn reported that the patient's medical records showed that she did not report the odorous discharge until after her second delivery.
VERDICT:
A New York $50 million verdict was returned.
Related article:
Management of wound complications following obstetric anal sphincter injury (OASIS)
Abdominal wall hematoma during pregnancy: $2.5M award
At 35 weeks' gestation, a 38-year-old woman presented to the emergency department (ED) with right upper abdominal pain. Her pregnancy was at high risk because of her age and the fact that she had thrombophilia involving both factor V and protein S deficiency. During pregnancy she was anticoagulated. She had been coughing from bronchitis, which was treated with antibiotics and an inhaler.
In the ED, laboratory testing determined that her blood was not properly clotting. Upper abdominal ultrasonography (US) showed an abdominal wall hematoma and gall stones. The ED physician, after contacting the on-call ObGyn, told the patient that nothing further could be done until after the baby's birth and prescribed medications for nausea and pain. The patient was discharged.
Thirty-three hours later, the patient was rushed to the hospital after she was found barely responsive, pale, and in severe pain. US results showed that the hematoma had grown extensively. The patient was in hypovolemic shock having lost more than 50% of her blood volume. She was admitted to the intensive care unit.
After induced labor, a stillborn son was delivered. The autopsy report revealed that the child died from either asphyxiation or an hypoxic ischemic event that occurred when the mother went into shock.
PATIENT’S CLAIM:
The ED physician and staff were negligent. Once the hematoma was identified, the standard of care is to monitor the hematoma with regular US. Instead, the ED physician discharged the patient. The ED physician contacted the on-call ObGyn but did not ask for a consult. The patient should have been admitted for monitoring.
DEFENDANT'S DEFENSE:
The ED physician met the standard of care. The mother's condition would likely have been detected during a nonstress test scheduled for the following day but the mother missed the prenatal exam because she had just left the hospital.
VERDICT:
A $2.5 million Missouri verdict was returned.
Incorrect due date, child with brain injuries: $1.2M
When a pregnant woman presented for her first prenatal visit, she was unsure of the date of her last menstrual period. During subsequent prenatal visits, she underwent 3 ultrasounds.
Labor was induced on August 1 because she reported gastrointestinal reflux. The infant appeared healthy at birth but soon went into respiratory distress. He was slow to meet developmental goals and was believed to be autistic. At age 5 years, he was given a diagnosis of periventricular leukomalacia.
PARENT’S CLAIM:
The child, 11 years old at the time of trial, has permanent brain injuries due to premature delivery. The mother's due date should have been projected as August 25 according to prenatal US measurements. The ObGyn misinterpreted the US data and estimated a due date of August 15. Therefore induction on August 1st caused him to be premature.
PHYSICIAN’S DEFENSE:
The standard of care was met. Gestational age evaluation using US is an estimate based on the child's size at specific time points, not an exact calculation, especially if the mother is not sure about the date of her last menses.
VERDICT:
A $1.2 million New Jersey verdict was returned.
Related article:
Three good apps for calculating the date of delivery
Bacterial infection blamed for birth injury
A woman was at 28 weeks' gestation when her membranes ruptured on September 28. She began to leak amniotic fluid and was put on bed rest. She saw her ObGyn on October 13 with signs of a bacterial infection of her membranes. The ObGyn decided to induce labor; a baby girl was born 11 hours later. The child had meningitis at birth and other infection-related complications including a brain hemorrhage. She continues to have permanent neurologic deficits.
PARENT’S CLAIM:
The ObGyn was negligent in not immediately delivering the child via cesarean delivery on October 13. The delay exposed the baby to infection for 11 more hours; the extended exposure led to her permanent injury.
PHYSICIAN’S DEFENSE:
The patient's treatment met the standard of care.
VERDICT:
A Virginia defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.

