In the U.S., mefenamic acid was one of the first drugs approved for dysmenorrhea, and clinical studies have shown meclofenamate to be very effective in improving symptoms and altering the underlying pathophysiology.36,37 The dual mechanism of action likely gives these agents an edge in efficacy, although no clinical trials have been initiated to evaluate this presumed advantage. Intrauterine pressure changes have been documented as soon as 15 minutes after administration of the medications, suggesting a very rapid onset of action (obviating the need for preloading). In addition, in vitro studies have demonstrated meclofenamate’s ability to inhibit the activity of 5-lipooxygenase, unlike members of the propionic acid group, which have little or no inhibitory ability.38,39 The clinical significance of inhibiting the production of the extremely potent leukotrienes has yet to be fully explored.
TABLE 1
Families of NSAIDs
| Family | Example |
|---|---|
| ENOLIC ACIDS | |
| PYRAZOLONES | |
| Oxyphenbutazone | Azolid** |
| Phenylbutazone | Butazolidin** |
| Nabumetone | Relafen |
| Celecoxib | Celebrex |
| Rofecoxib* | Vioxx |
| OXICAMS | |
| Piroxicam | Feldene, Piroxicam |
| Meloxicam | Mobic |
| CARBOXYLIC ACIDS | |
| SALICYLIC ACIDS | |
| Acetylsalicylic acid | Aspirin (various) |
| Diflunisal | Dolobid |
| Salicylate | Disalcid, Trilisate |
| INDOLEACETIC ACIDS | |
| Diclofenac potassium | Cataflam |
| Diclofenac sodium | Voltaren, Arthrotec (combined with misoprostol) |
| Etodolac | Lodine |
| Indomethacin | Indocin |
| Ketorolac tromethamine | Acular, Toradol |
| Sulindac | Clinoril, Sulindac |
| Tolmetin | Tolectin, Tolmetin |
| PROPIONIC ACIDS | |
| Fenoprofen calcium | Fenoprofen |
| Flurbiprofen | Flurbiprofen |
| Ibuprofen* | Motrin |
| Ketoprofen | Orudis, Oruvail, Ketoprofen |
| Naproxen sodium* | Aleve, Anaprox, Naprelan |
| Naproxen* | Naprosyn |
| FENAMATES | |
| Meclofenamate sodium* | Meclofenamate |
| Mefenamic acid | Ponstel |
| *FDA-approved for primary dysmenorrhea | |
| **No longer available | |
| Adapted from: Smith RP.Gynecology in Primary Care. Baltimore, Md: Williams and Wilkins; 1996:399. | |
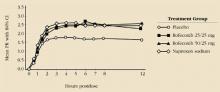
FIGURE 1 Comparison of rofecoxib, naproxen, and placebo in treatment of primary dysmenorrhea
Reprinted with permission from The American College of Obstetricians and Gynecologists. Morrison BW, Daniels SE, Kotey P, Cantu N, Seidenberg B. Rofecoxib, a specific cyclooxygenase-2 inhibitor, in primary dysmenorrhea: a randomized-controlled trial. Obstet Gynecol. 1999;94:504-508.
COX-2 inhibitors
Although the short-term efficacy and safety of new selective COX-2 inhibitors appear to be good, several concerns remain. Despite a decrease in the incidence of GI side effects with these agents, their use by patients with active GI ulceration, infection with Helicobacter pylori, or inflammatory bowel disease has not been adequately studied. Indeed, recent studies suggest that, at therapeutic concentrations, no NSAID—not even the selective COX-2 inhibitors—completely eliminates gastric cyclooxygenase activity.40
In addition, questions have been raised about the speed and efficacy of the selective COX-2 inhibitors for the management of acute pain, compared with conventional NSAIDs.41 When used for postoperative analgesia, these agents theoretically could retard wound healing because of the role that COX-2 plays in healing and neovascularization. As more data emerge about the physiologic functions of COX-1 and -2 (Table 2), there are growing concerns that COX-2 is not restricted to inflammation and pathology, suggesting the possibility of unanticipated adverse effects associated with its use. For example, there is evidence of constitutive expression of COX-2 in the kidney and brain, and essential physiological functions in ovulation and implantation.42 In the treatment of dysmenorrhea, the increased cost of these drugs over the more commonly used agents, along with the lack of clinical efficacy studies, suggests a second-line role.
Like most NSAIDs, COX-2 inhibitors fall into pregnancy category C. Because of the risk of premature closure of the ductus arteriosus, they should not be used in the third trimester of pregnancy. In addition, drug levels in human milk mimic those in serum, so the decision to use these agents in nursing mothers must be made carefully.
Studies over the past 10 years have revealed that the cyclooxygenase enzyme (COX) is found in 2 isomeric forms, known as COX-1 and COX-2.1 Initial investigations suggested that COX-1 was present in most tissues and responsible for the homeostatic production of arachidonic acid metabolites. The COX-2 enzyme was thought to be induced in response to inflammatory stimuli such as cytokines and bacterial lipopolysaccharides, rather than expressed under normal cellular function. Thus, the COX-2 form was thought to be responsible for the large amounts of prostaglandins associated with inflammation. It was further hypothesized that COX-2 used intracellular arachidonic acid as a substrate almost exclusively, while COX-1 could use phospholipase A2 as an extracellular substrate under some conditions.2
Recent data suggest that COX-1 and -2 are more complex than originally assumed. There is increasing evidence that COX-2 is constitutively expressed in the brain, kidneys, and pancreatic islet cells and plays a role in intestinal tolerance to dietary antigens, ulcer healing, ovulation, and implantation. Transgenic mice with deletions of the COX-2 enzyme maintain the inflammatory response when only COX-1 is present.3
In the reproductive tract, COX-2 expression increases substantially in midcycle because of the surge in luteinizing hormone (LH). COX-2 and the resulting prostaglandins (released from granulosa cells) are thought to play an important role in rupture of the follicle.4,5 With fertilization, COX-2 expression increases in the endometrium surrounding the implantation site.6 The resultant prostaglandins are important for successful implantation and angiogenesis. Interestingly, transgenic mice that lack the COX-2 enzyme are infertile, while those missing only the COX-1 enzyme have normal reproduction.7,8
Studies also have demonstrated a rapid increase in COX-2 expression in the placenta and amnion immediately before and during labor.9 It is well established that prostaglandins have a pivotal role in myometrial contraction10 and inhibition of COX-2 has been shown to delay labor.11
The COX-1 and -2 enzymes share approximately 60% homology.12 Both have a long, narrow channel that is the active site of arachidonic acid folding and oxygenation. The critical difference between the 2 isoenzymes occurs at position 523, where the COX-1 enzyme has an isoleucine while COX-2 has a valine.13 This substitution causes the channel in the COX-2 form to be 17% wider; it also provides a side pocket that increases the volume of the active site by 8%. Drugs that are designed to block the COX-2 enzyme take advantage of this difference in channel size—they are too large to fit the normal channel. Nonselective NSAIDs are small enough to block the channel in both isoenzymes while, at least in theory, the selective agents can block only the larger channel.14 Most COX-2 inhibitors also exhibit some action against the COX-1 isoform.—Roger P. Smith, MD, and Jeffrey Ellis, MD
REFERENCES
1. Smith WL, Garavito RM, DeWitt DL. Prostaglandin endoperoxide H synthase (cyclooxygenase)-1 and -2. J Biol Chem. 1996;271:33157.-
2. Herschman HR. Prostaglandin synthase 2. Biochem Biophys Acta. 1996;1299:125-140.
3. Wallace JL, Bak A, McKnight W, Asfaha S, Sharkey KA, MacNaughton WK. Cyclooxygenase 1 contributes to inflammatory responses in rats and mice: implications for gastrointestinal toxicity. Gastroenterology. 1998;115:101-109.
4. Richards JS, Fitzpatrick SL, Clemens JW, Morris JK, Alliston T, Sirois J. Ovarian cell differentiation: a cascade of multiple hormones, cellular signals, and regulated genes. Recent Prog Horm Res. 1995;50:223-254.
5. Akil M, Amos RS, Stewart P. Infertility may sometimes be associated with NSAID consumption. Br J Rheumatol. 1996;35:76-78.
6. Chakraborty I, Das SK, Wang J, Dey SK. Developmental expression of the cyclo-oxygenase-1 and cyclooxygenase-2 genes in the peri-implantation mouse uterus and their differential regulation by the blastocyst and ovarian steroids. J Mol Endocrinol. 1996;16:107-122.
7. Lim H, Paria BC, Das SK, Dinchuk JE, Langenbach R, Trzaskos JM, et al. Multiple female reproductive failures in cyclooxygenase 2-deficient mice. Cell. 1997;91:197-208.
8. Langenbach R, Loftin C, Lee C, Tiano H. Cyclooxygenase knockout mice: models for elucidating isoform-specific functions. Biochem Pharmacol. 1999;58:1237-1246.
9. Gibb W, Sun M. Localization of prostaglandin H synthase type 2 protein and mRNA in term human fetal membranes and decidua. J Endocrinol. 1996;150:497-503.
10. O’Brien WF. The role of prostaglandins in labor and delivery. Clin Perinatol. 1995;22:973-984.
11. Mitchell MD, Romero RJ, Edwin SS, Trautman MS. Prostaglandins and parturition. Reprod Fertil Dev. 1995;7:623-632.
12. Kurumbail RG, Stevens AM, Gierse JK, et al. Structural basis for selective inhibition of cyclooxygenase-2 by anti-inflammatory agents. Nature. 1996;384:644-4.(Published correction appears in Nature. 1997;385:555.)
13. Gierse JK, McDonald JJ, Hauser SD, Rangwala SH, Koboldt CM, Seibert K. A single amino acid difference between cyclooxygenase-1 (COX-1) and -2 (COX-2) reverses the selectivity of COX-2 specific inhibitors. J Biol Chem. 1996;271:15810.-
14. Lanzo CA, Beechem JM, Talley J, Marnett LJ. Investigation of the binding of isoform-selective inhibitors to prostaglandin endoperoxide synthases using fluorescence spectroscopy. Biochemistry. 1998;37:217-226.