Delivery of the shoulders often gets overlooked in discussions
of episiotomy
(Comment & Controversy, November 2012)
Difficult fetal extraction at cesarean delivery:
What should you do?
Robert L. Barbieri, MD (Editorial, January 2012)
What is the significance of the head-to-body delivery interval
in shoulder dystocia?
William A. Grobman, MD, MBA (Examining the Evidence, December 2011)
Does the use of multiple maneuvers in the management of shoulder dystocia increase the risk of neonatal injury?
Robert B. Gherman, MD (Examining the Evidence, August 2011)
CASE: Shoulder dystocia resulting in persistent injury to C5 and C6
A 30-year-old, G2P1 woman presented in labor at 39 weeks and reported a strong desire to have a natural childbirth. She was taking insulin for gestational diabetes mellitus diagnosed in the second trimester. Her body mass index was 43 kg/m2, and her height was 4 ft 11 in. The estimated fetal weight was 9 lb. She had a prior vaginal delivery. During her antepartum care the patient was extensively counseled about the risk of shoulder dystocia and obstetric brachial plexus (OBP) injury.
The patient progressed normally through labor without anesthesia. At birth, the baby delivered occiput posterior and restituted to right occiput transverse. There was a turtle sign, and the obstetrician diagnosed a shoulder dystocia, called for help, and told the mother to stop pushing. An attempt to deliver the fetal head with gentle downward guidance was unsuccessful. The McRoberts maneuver and suprapubic pressure combined with gentle downward guidance on the fetal head did not result in delivery. A mediolateral episiotomy was made and the Rubin and Wood maneuvers were attempted without success. The obstetrician then successfully delivered the posterior arm and the body of the baby was easily delivered.
The shoulder dystocia lasted 2 minutes before successful delivery. The Apgar scores were 3 and 6 at one and five minutes, respectively. The umbilical cord artery pH was 7.18. The birthweight was 9 lb 2 oz. A diagnosis of OBP injury involving C5 and C6 was made. At discharge the OBP injury persisted.
What is OBP injury?
Shoulder dystocia, which affected this mother and fetus, is a problem involving the impaction of the fetal shoulder behind the maternal symphysis pubis. Shoulder dystocia is a “bony problem.” Although shoulder dystocia cannot be predicted reliably, risk factors include:
- fetal macrosomia
- maternal diabetes
- maternal weight gain
- prepregnancy obesity
- multiparity
- operative vaginal delivery.1-3
The injury can be serious and permanent. The feared consequence of shoulder dystocia is permanent obstetric brachial plexus injury and/or fetal neurologic damage caused by reduced cord blood flow and fetal asphyxia. Occasionally, shoulder dystocia results in fetal death.
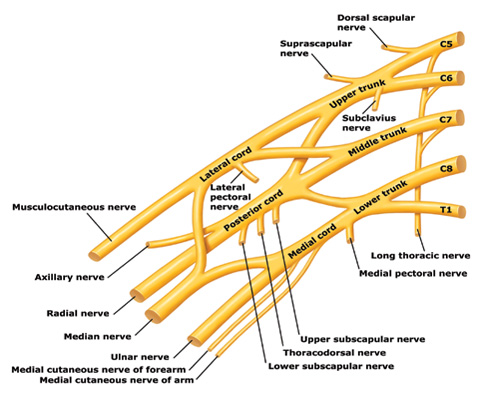
Trunks and cords of the brachial plexus
C5 and C6 roots merge to form the upper trunk, C7 root forms the middle trunk, and C8 and T1 roots merge to form the lower trunk.
How can an OBP injury occur?
Most cases are unilateral and arise when one or more of the brachial plexus nerves ( Figure ) are compromised. The forces of labor, fetal position, maternal pushing, and force applied to the fetal head and neck by a clinician all may contribute to an OBP injury.4 It is important to note that up to one-third of all OBP injuries occur in births not associated with a recognized shoulder dystocia.5
Erb’s palsy. Injuries to the C5 and C6 nerves account for about 50% of cases. The muscle groups impacted by this injury include the deltoid and infraspinatus muscles (mainly C5) and the biceps muscle (mainly C6). This pattern results in an adducted and internally rotated upper arm, an extended forearm, with preservation of hand and wrist movement.
Erb’s palsy plus. Injury to C5, C6, and C7 nerves accounts for about 35% of cases and manifests as adduction and internal rotation of the arm, extension and pronation of the forearm, plus flexion of the wrist and fingers—the so-called waiter’s tip posture.
Klumpke’s palsy. Isolated injury to the C8 nerve and T1 root occurs infrequently and manifests as isolated hand paralysis and Horner’s syndrome.
Approximately one in five OBP injuries persist for years following birth. The incidence of OBP injury ranges from 1.0 to 3.0 cases per 1,000 births.6-8 In a review of studies with at least 3 years of follow-up and less than 10% loss to follow-up, the authors reported that the three best studies observed a risk of persistent OBP of 10%, 19%, and 27%.9
Long-term management of OBP injury
The optimal approach to management of OBP injury is unknown because few high-quality studies are available to guide therapy. Typically, 3 to 9 months of observation and physical therapy are recommended following birth, with the hope that the majority of newborns will recover some or almost all function. Physical therapy is focused on reducing the occurrence of joint contractures and maintaining range of motion in the shoulder, elbow, wrist, and fingers.


