Myomectomy is the surgery of choice for women who have symptomatic fibroids and who wish to retain their uterus. And laparoscopic myomectomy is preferable to the abdominal approach in many ways, offering: 1-4
- faster recovery
- a shorter hospital stay
- diminished blood loss
- decreased adhesion formation
- a comparable or higher rate of pregnancy.
Nevertheless, laparoscopic myomectomy is a technically challenging procedure with surgeon-specific limitations. The biggest challenge: appropriately suturing the hysterotomy site.
In this article, I share my experience with laparoscopic myomectomy and offer 8 pearls that may contribute to a successful outcome.
1. Don't settle on laparoscopy prematurely
Given its advantages over the abdominal route, laparoscopic myomectomy should be the preferred approach in the treatment of symptomatic uterine fibroids ( FIGURE 1 ). However, not all patients are appropriate candidates for laparoscopy. Several guidelines have recommended a maximum number and size of fibroids for laparoscopic removal, but practice varies widely, and experienced surgeons successfully take on cases that are well beyond the limits set by most published guidelines.5-7
At our institution, we do not have firm guidelines in place for the number and size of fibroids that can be removed laparoscopically. Other variables enter into decision-making and counseling, among them any medical comorbidity or history of uterine surgery the patient may have, as well as her desires in regard to childbearing and uterine retention.
Hysterectomy may be the most straightforward option for women who have symptomatic fibroids and who have completed childbearing. However, myomectomy is also appropriate as long as the patient is aware of the risk that fibroids may recur and the potential for further surgery. When the patient is in her late 40s or early 50s, the likelihood of fibroid recurrence may be lower than it is in the general population.
In my practice, submucosal and intracavitary fibroids smaller than 4 cm and more than 5 mm away from the uterine serosa are generally removed hysteroscopically, an approach beyond the scope of this article. In women who have completed childbearing but who wish to conserve the uterus, we deliberately enter the uterine cavity laparoscopically because this strategy allows for efficient removal of submucosal and intracavitary fibroids.
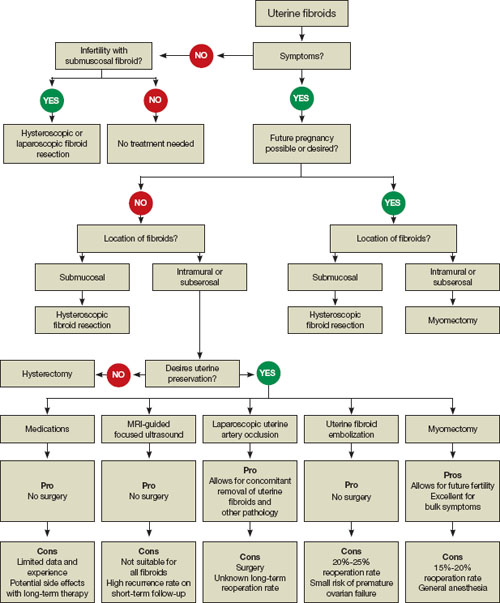
FIGURE 1 When and how to treat uterine fibroids
2. Estimate the duration of surgery
When the patient has fibroids that are intramural or subserosal, our general rule of thumb is to determine her suitability for laparoscopic myomectomy, based on the estimated duration of the operation. A surgeon's ability to calculate the length of the operation for a particular patient increases with experience.
We tend to recommend the laparoscopic approach when the procedure is expected to take less than 3 hours to complete. More than 95% of our patients fall into this category.
When we anticipate a prolonged operating time, we discuss the option of hand-assisted laparoscopic myomectomy. This approach involves two or three 5-mm trocar punctures high on the abdomen in conjunction with a suprapubic incision, 6 to 7 cm in length with a hand port in place. Prospective studies have demonstrated a significantly longer recovery with minilaparotomy than with laparoscopy, but these trials compared uteri of similar size.4,8 We expect the laparoscopic approach to confer fewer advantages when operative time is prolonged significantly.
In our practice, we consider one or more of the following conditions appropriate for hand-assisted laparoscopic myomectomy:
- a very large uterus (i.e., heavier than 1,500 to 2,000 g). In these cases, operating times can be excessive because of the need for extensive suturing and morcellation, and bleeding may increase as a result
- more than 20 fibroids on magnetic resonance imaging (MRI). It can be a challenge to locate all of the fibroids; multiple uterine incisions may be necessary
- a medical comorbidity that renders the patient unable to tolerate prolonged anesthesia. For example, we operated on a patient who had Ehlers-Danlos syndrome and who needed to avoid a prolonged operation due to fragile bones and joint laxity.
Of necessity, these guidelines will vary from practice to practice, and gynecologic surgeons who are just beginning to perform laparoscopic myomectomy should not include multiple fibroids or a large uterus among their initial cases. Instead, perform the first few cases in patients who have not had abdominal surgery and who have a symptomatic intramural or subserosal fibroid that is close to the uterine fundus and no larger than 6 cm in diameter.

