CASE: New-onset abdominal pain and a history of bariatric surgery
A 28-year-old woman who is 14 weeks pregnant (G5P1A4) complains of abdominal pain, nausea, and vomiting for the past 3 days. Four years ago, she underwent a successful Roux-en-Y gastric bypass, and her body mass index (BMI) decreased from 61.1 to 34.8 as a result. Today, after unremarkable ultrasonography at an outside hospital, she is transferred to your facility, where she is noted to be afebrile and tachycardic (133 bpm) with a very tender abdomen and a white blood cell (WBC) count of 12.2×103/μL.
Could her symptoms be related to her history of gastric bypass? How should you manage her condition?
This case illustrates why it is imperative that Ob Gyns have a basic understanding of bariatric surgery—particularly the types of procedures being performed today and the complications that may arise.
In this case, urgent intervention is called for, given the elevated WBC count and extreme tenderness of the abdomen. This patient was taken to surgery without waiting for additional imaging studies. Operative findings included intussusception with necrosis, a late complication of the Roux-en-Y procedure, necessitating resection of 60 cm of small intestine ( FIGURE 1 ). Although fetal heart sounds remained encouraging overnight, fetal demise occurred the next day. The patient’s physical recovery was otherwise unremarkable.
This scenario is not as unlikely as you might imagine. A similar episode was described in 2004.1 The outcome: maternal and fetal death.

FIGURE 1 Life-threatening intestinal obstruction
Patchy and continuous necrosis is evident following reduction of an obstruction-causing intussusception.
A boom in bariatric surgery
The incidence of surgical weight-loss procedures increased sixfold over a recent 7-year time span.2 In 2008 alone, more than 200,000 people underwent this type of operation—at least half of them women of reproductive age.2,3 In my experience at the University Hospitals of Cleveland Bariatric Program, which I directed, 85% of patients were women.4 This percentage is similar to the gender breakdown in other bariatric programs.
Because you are called on to provide both primary and specialty care, you are very likely to encounter women who have undergone bariatric surgery or who are considering it. As the prevalence of morbid obesity continues to rise, so will the need for familiarity with surgical weight-loss reduction.
In this article, I offer an overview of bariatric surgery, focusing on:
- the different procedures performed today
- the potential complications associated with the most common operations
- the need for nutritional assessment.
In the process, I discuss the health benefits of bariatric surgery, including greater fertility and improved pregnancy outcomes.
How we talk about obesity
The language of obesity centers on a basic metric: the body mass index (BMI).5 This index was devised in the 19th century by Adolphe Quetelet to describe total body fat.
Consider its use to describe two markedly overweight individuals. One stands 6 ft and weighs 500 lb; the other stands 5 ft and weighs 400 lb. It is obvious which person is heavier; the BMI quantifies who is actually bigger. The first individual has a BMI of 67.8, whereas the shorter person has a BMI of 78, despite weighing 100 lb less.
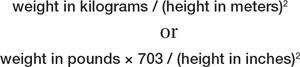
The formula for determining BMI is:
Among the imperfections of the BMI are its failure to differentiate between genders and its marked inaccuracy in persons who have significant muscle mass and limited body fat, such as body builders. However, it does make it possible to compare patients of different height and weight, thereby facilitating attempts to prognosticate the risk of illness and identify candidates for bariatric surgery ( TABLE 1 ).
The 1991 National Institutes of Health (NIH) Consensus Conference on Gastrointestinal Surgery for Severe Obesity recommended that bariatric surgery (restrictive and bypass procedures) be considered for patients who have a BMI of 40 or above and for patients who have a BMI of 35 or above with high-risk comorbidity.6

