Surgical Techniques
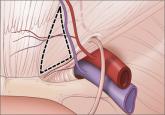
Anatomy for the laparoscopic surgeon
Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations...

Notable judgments and settlements
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
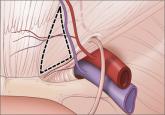
Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations...
It is higher after elective primary cesarean.
How to prevent recurrent urinary tract infection in sexually active premenopausal women, postmenopausal patients, and women undergoing pelvic...
