DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
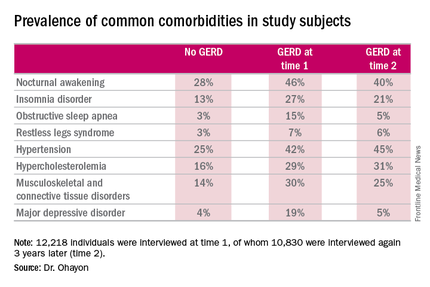
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.