An important new initiative to reclassify psychiatric medications is underway. Currently, psychotropic drugs are named primarily for their clinical use, usually as a member of 1 of 6 classes: antipsychotic, anti‑depressant, mood stabilizer, stimulant, anxiolytic, and hypnotic.1,2
This naming system creates confusion because so-called antidepressants commonly are used as anxiolytics, antipsychotics increasingly are used as antidepressants, and so on.1,2
Vocabulary based on clinical indications also leads to difficulty in classifying new agents, especially those with novel mechanisms of action or clinical uses. Therefore, there is a need to make the names of psychotropic drugs more rational and scientifically based, rather than indication-based. A task force of experts from major psychopharmacology societies around the world is developing an alternative naming system that is increasingly being accepted by the major experts and journals throughout the world, called Neuroscience-based Nomenclature (NbN).3-5
So, what is NbN?
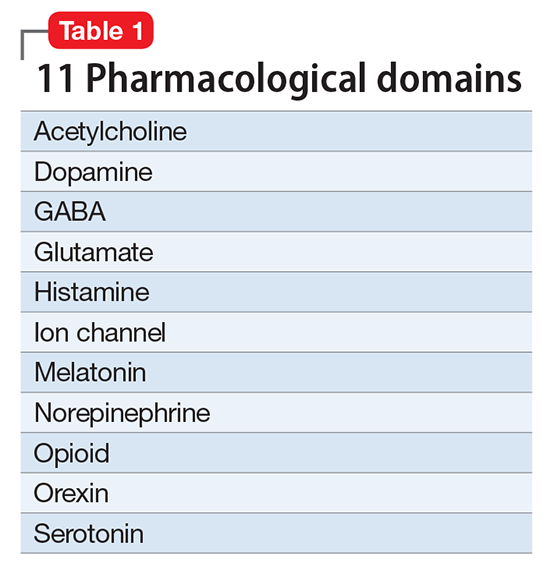
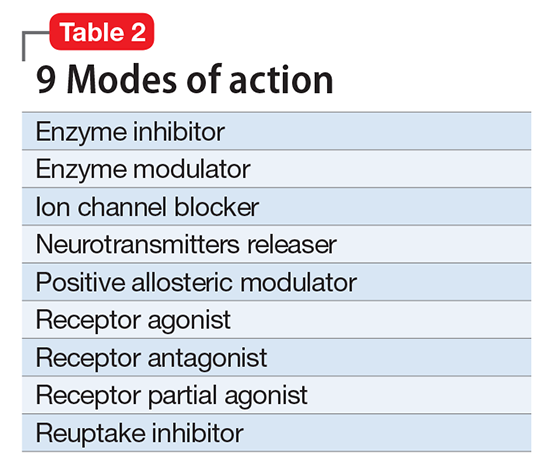
First and foremost, NbN renames the >100 known psychotropic drugs by 1 of the 11 principle pharmacological domains that include well-known terms such as serotonin dopamine, acetylcholine, and GABA (Table 1). Also included in NbN are 9 familiar modes of action, such as agonist, antagonist, reuptake inhibitor, and enzyme inhibitors (Table 2).3-5
NbN has 4 additional dimensions or layers3-5:
- The first layer enumerates the official indications as recognized by the regulatory agencies (ie, the FDA and other government organizations).
- The second layer states efficacy based on randomized controlled trials or substantial, evidence-based clinical data, as well as side effects (not the exhaustive list provided in manufacturers’ package inserts, but only the most common ones).
- The third layer is comprised of practical notes, highlighting potentially important drug interactions, metabolic issues, and specific warnings.
- The fourth section summarizes the neurobiological effects in laboratory animals and humans.
Specific dosages and titration regimens are not provided because they can vary among different countries, and NbN is intended for nomenclature and classification, not as a prescribing guide.
How does it work in practice?
Major journals in the field have begun adapting NbN for their published papers and Current Psychiatry is joining them. Specifically, journals adapting NbN will require authors to clarify the meaning of terms they use for drugs by defining as “antipsychotic,” for example, along with the NbN term (eg, dopamine D2 antagonist) where the drug name first appears in the paper. To make all new papers searchable by NbN terminology, the NbN of the drugs that the paper covers should be added to the keywords of the paper. The new keywords will include those relevant 11 pharmacological domains and 9 modes of action of the drugs discussed in the paper, which will make the process easier for authors and readers searching for drugs in our publications. To “translate” between old and new nomenclature, the easiest and recommended way is to use the free NbN app, which is available on the project’s Web site (http://nbnomenclature.org), as well as Google Play and iTunes. We recommend that journal editors include in their author instructions a link to the glossary that illustrates NbN in practice (http://nbnomenclature.org/authors).
What is the current status?
Two international organizations endorse NbN, and the chief editors of nearly 3 dozen scientific journals, including Current Psychiatry, support the development of this classification system for eventual implementation within the scientific literature. Presentations at symposia at international meetings also have taken place or are ongoing, including a scientific session at the 2016 American Psychiatric Association (APA) annual meeting and another planned for the Presidential Symposium at 2017 APA annual meeting; other presentations are scheduled at the American College of Neuropsychopharmacology in December 2017 and the European College of Neuropsychopharmacology in September 2017.
Clinicians should start adopting the NbN for the psychotropic drugs they prescribe every day. It is more scientific and consistent with the mechanism of action than with a specific disorder because many psychotropic medications have been found to be useful in >1 psychiatric disorder.