In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
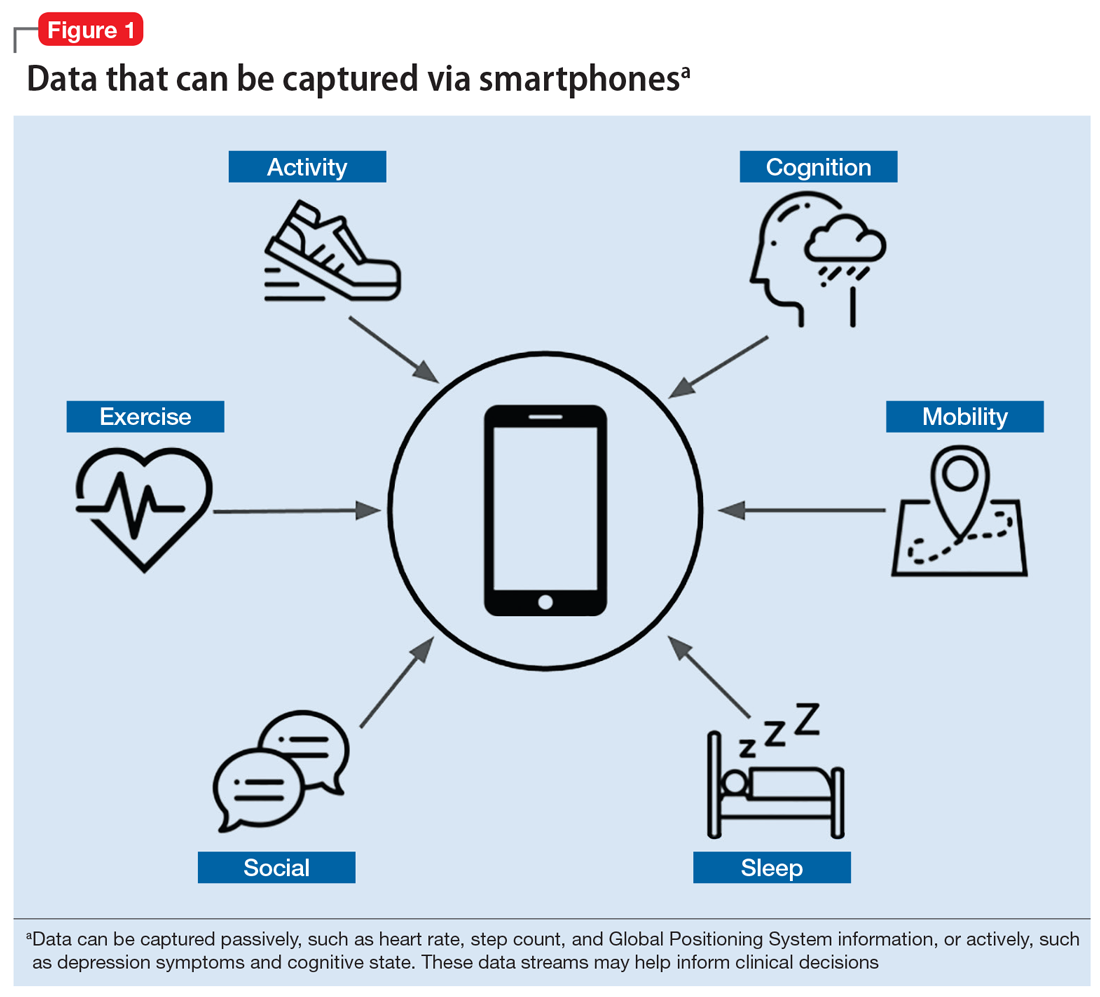
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...