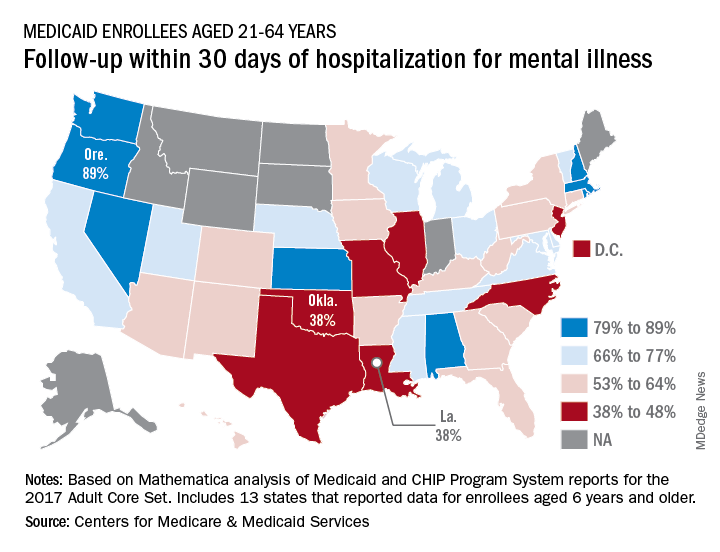
Follow-up rates after hospitalization for mental illness varied considerably among the states, ranging from 38% to 89% in 2016, according to the Centers for Medicare & Medicaid Services.
All that variation added up to a national median of 64% of Medicaid enrollees who saw a mental health clinician within 30 days of discharge, CMS reported in its Medicaid and Children’s Health Insurance Program Scorecard.
The other states in the top five were Nevada (85%), Rhode Island (82%), and New Hampshire (80%), scoreboard data show.
In Louisiana and Oklahoma, the states with the lowest rate, only 38% of Medicaid enrollees had a follow-up visit within 30 days of their discharge. The next three rungs on the follow-up ladder were occupied by New Jersey (43%), Illinois (44%), and North Carolina (44%), the CMS said after a recent refresh of data in the scorecard.
“Everyone – whether you are a beneficiary, taxpayer, or lawmaker – deserves to understand the performance of our nation’s largest health coverage programs and often the largest state expenses,” CMS Administrator Seema Verma said in a written statement. “More and more states are voluntarily reporting their health outcomes in the scorecard, and the new data is leading us into an era of increased transparency and accountability, so that together we can improve the quality of care we give to the vulnerable Americans that depend on this vital program.”
Data for this measure “reflect state reporting for Medicaid enrollees ages 21 to 64” years, the CMS noted, but eight states did not report at all. A total of 13 states reported on enrollees aged 6 years and older, 2 states reported results for those aged 21 and older, and 1 state reported data for ages 6-64.
“The included populations … can vary by state. For example, some states report data on certain populations such as those covered under managed care but not those covered under fee for service. This variation in data can affect measure performance and comparisons between states,” the CMS said.