Greater use of electronic health records would cut greenhouse gas emissions, energy use, waste and toxic chemical production, and water consumption, according to a study by Marianne C. Turley, Ph.D., and her associates at Kaiser Permanente.
Even after factoring in the additional energy consumption from the increased use of personal computers, the overall net effect on the environment would be favorable, the researchers concluded based on an analysis of the impact of the Kaiser Permanente EHR system, which covers 8.7 million beneficiaries.
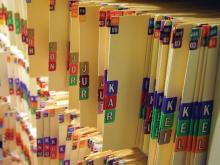
Annually, the use of the Kaiser EHR system eliminated the use of 1,373 tons of paper by discontinuing the use of paper medical charts, x-ray jackets, and administrative forms. The system also decreased annual gas consumption by an estimated 3.3-10 million gallons by cutting the number of visits by 4-13 million. Patients who were registered online could correspond with their providers about nonemergency concerns through secure e-mail messages, the investigators reported (Health Aff. 2011;30:938-46).
Switching from desktop to laptop computers saved 89,300 megawatt hours and digitizing x-rays eliminated the waste of 203 tons of plastic and 79 tons of toxic chemicals. Using the Environmental Protection Agency’s greenhouse gas equivalencies calculator, Dr. Turley and her associates estimated that Kaiser’s efforts reduced greenhouse gas emissions by 9,200 tons.
Results were based on data from regional operational reports, paper-purchasing records, and internal pharmaceutical reports. Travel distance was estimated by calculating the distance from patient addresses to Kaiser-participating primary care buildings and aggregating them by region.
With a growing emphasis on health technology, the Kaiser study showed that "the use of electronic health records can both change the face of health care and help reduce its environmental footprint," the researchers wrote.
Despite these findings, Dr. Turley and her associates said that the environmental impact of switching to electronic health records will vary from system to system. As the Affordable Care Act calls for implementation of electronic systems, they said further analysis is necessary to determine the impacts of widespread implementation.
Although 51% of office-based physicians are currently using an electronic system, only 10% of practices reported their systems as being fully functioning, according to the most recent evaluation from the Centers for Disease Control and Prevention. Regardless, implementation of electronic systems will probably increase as provisions in the American Recovery and Reinvestment Act of 2009 create incentives for providers who invest in electronic systems. Public and private investment in these systems is expected to reach $40 billion in the next several years, according to the investigators.