Alternative agents are widely used and warrant study. Those shown to be safe can be used alone or with other therapies, but advise the patient that these agents may not be effective. Relaxation and exercise may decrease hot flashes,22 although some outcomes have been similar to a placebo response.
SLEEP APNEA AT PERIMENOPAUSE
Obstructive sleep apnea (OSA), although more common in men than women, appears to increase during perimenopause. Women with untreated OSA are twice as likely as men to be treated for depression, less likely to report excessive daytime sleepiness and snoring, and more likely to present with depression, anxiety, and morning headache.
Bixler et al23 interviewed 12,219 women and 4,364 men ages 20 to 100 and conducted 1-night sleep studies in 1,000 women and 741 men. OSA rates were 3.9% in men, 0.6% in premenopausal women, 2.7% in postmenopausal women not taking HRT, and 0.5% in postmenopausal women taking HRT.
The risk of sleep-disordered breathing is lower during early menopause and peaks at approximately age 65. Declining hormones likely play a role; progesterone increases ventilatory drive, and estrogen increases ventilatory centers’ sensitivity to progesterone’s stimulant effect. In small studies, exogenous progesterone has shown a slight effect in improving OSA.24
OSA’s transient, repetitive upper airway collapse increases inspiratory effort and may cause hypoxemia. Repeated arousals can lead to prolonged awakenings and unrefreshing sleep. Snoring and increased body mass index are strongly associated factors, although the Wisconsin Sleep Cohort Study10 showed an increase in sleep apnea in perimenopausal women that was unrelated to increased body mass index.
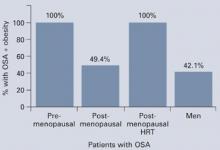
Obesity may not explain the increase in obstructive sleep apnea at perimenopause (Figure 3),28 although body fat distribution does change with aging. Women at perimenopause are likely to develop abdominal weight distribution.
Figure 3 Increased OSA in postmenopausal women is unrelated to obesity (BMI >32)
Obstructive sleep apnea (OSA) in 1,000 women and 741 men was associated exclusively with obesity in premenopausal women and postmenopausal women using HRT, but nearly one-half of the postmenopausal women with OSA were not obese.
Source: Adapted from reference 23.Treatment. In the Sleep Heart Health Study25 of 2,852 women age 50 or older, HRT users had one-half the apnea prevalence of nonusers (6% vs 14%). HRT users were less likely to awaken at night and to get inadequate sleep. Snoring rates were similar (25% for HRT users, 23% for nonusers).
Nasal continuous positive airway pressure (CPAP) is the mainstay of apnea treatment, although some women appear to have difficulty accepting CPAP.26 Weight loss and moderate exercise can help manage weight and improve sleep quality by increasing slow-wave sleep. Regular exercise also may improve depressed mood.
Related resources
- American College of Obstetricians and Gynecologists. www.acog.org
- The North American Menopause Society. www.menopause.org
Drug brand names
- Conjugated estrogens • Premarin
- Eszopiclone • Lunesta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Medroxyprogesterone • Provera
- Micronized progesterone • Prometrium
- Mirtazapine • Remeron
- Trazodone • Desyrel
- Venlafaxine • Effexor
- Zaleplon • Sonata
- Zolpidem • Ambien
Disclosures
Dr. Krahn reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.