Oximetry provides only one or two types of data (oxygen saturation plus possibly heart rate), while other physiologic processes, e.g., body movement or sleep architecture, can repetitively be disrupted during sleep.
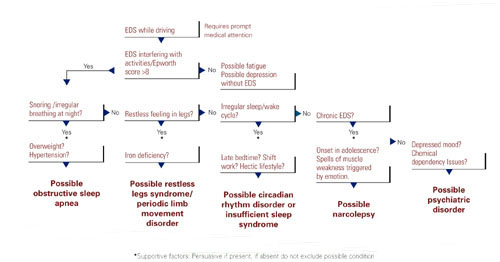
The most critical steps in detecting sleep disorders do not require technology or specialized expertise, but rather intuition and common sense. The psychiatrist should consider the possibility of a sleep disorder and incorporate pertinent questions into the clinical interview. Figure 1 lists sequential questions that might uncover specific sleep disorders. Once suspected, the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder detected.
Diagnosing and treating OSA
Recent epidemiologic studies show that OSA affects at least 4% of men and 2% of women in the United States.6 Psychiatrists are virtually assured of seeing patients with undiagnosed OSA. The condition is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because of sleep fragmented by frequent arousals.
Figure 1 THE SLEEPY PATIENT: Possible medical and psychiatric explanations
Obese patients are at higher risk than are patients at normal weight because of their body habitus. Alcohol or sedative medication use close to bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold, meaning that patients do not wake readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. New data associate OSA with multiple potential cardiovascular complications (arrhythmias, congestive heart failure, and myocardial infarction).7 Therefore, recognition and treatment are paramount.
The physical examination should focus on detecting nasal obstruction (having the patient sniff separately through each nostril can be helpful), big neck, crowded oropharynx (a low-hanging palate, reddened uvula, enlarged tonsils, large tongue size relative to oropharynx diameter) and jaw structure (particularly a small retrognathic mandible).
Referral for nocturnal polysomnography might be the next step. During a comprehensive sleep study, data is collected about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes (e.g., snoring, coughing) when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation are observed; these typically result in brief shifts in EEG frequency called arousals.
First-line interventions for OSA include avoidance of alcohol within 1 to 2 hours of bedtime, sleeping on the side instead of the back, weight loss (ideally with a regular exercise program), and nasal sprays for allergies.
If the first-line treatments for OSA are ineffective, nasal continuous positive airway pressure (CPAP) works well for almost all patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and the upper airway (Box 2). Some patients benefit from a brief trial of a sleeping medication, e.g., zolpidem or trazodone, for the first 1 to 2 weeks of nasal CPAP usage.

Nasal continuous positive airway pressure (CPAP) must be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent. CPAP can be started during the second half of a “split-night” sleep study after obstructive sleep apnea (OSA) has been diagnosed. Alternatively, the sleep laboratory might ask the patient to return for a second night for a trial of nasal CPAP.
Patients with severe OSA might notice improved sleep quality and reduced EDS, even after only a few hours of use. Such patients sometimes wish to start CPAP treatment immediately.
Overall, advances in masks and equipment have improved patient adherence to CPAP. Such innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many newer machines also have a data microchip that allows the clinician to determine the duration of usage, then use that information to counsel the patient about adherence if necessary.
Patient education also can promote CPAP adherence. Upon being first told they might need to sleep each night wearing a nasal mask, patients often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
As part of a comprehensive approach at the Mayo Sleep Disorders Center, patients watch an educational videotape, tour the sleep laboratory bedrooms before the sleep study, and are carefully fitted for masks. Ideally, the technologists interact with the patient during the sleep study to adjust the headgear and fine-tune other aspects of the equipment. The sleep specialist meets with the patient to compare the baseline diagnostic study results with changes in breathing patterns after a trial of nasal CPAP.
Other useful patient compliance tools include a CPAP informational handout, telephone access to nursing staff, and a 30-day follow-up visit.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner was likely the impetus for the appointment in the first place because of concerns about excessive snoring or apneas.
Image reprinted from Oct. 2001 Mayo Clinic Health Letter with permission of Mayo Foundation for Medical Education and Research, Rochester, MN 55905

