Table
Life-threatening effects of clozapine and their reported frequency of occurrence
| Adverse effect | Incidence rate among clozapine users |
|---|---|
| Agranulocytosis | 3/1000 person years* at 6 months |
| Hepatitis | Less than 1% |
| Hyperglycemia with ketoacidosis | Unknown, case reports |
| Myocarditis | 5.0-96.6 cases/100,000 patient years |
| Neuroleptic malignant syndrome | Unknown, several case reports |
| Orthostasis with cardiac collapse | 1/3,000 cases |
| Pulmonary embolism | 1/3,450 person years |
| Seizures | 5% after 1 year of therapy |
| * Person year = 1 person taking medication for 1 year | |
| Source: Clozaril prescribing information. In: Physicians’ Desk Reference (57th ed). Montvale, NJ: Thomson Healthcare, 2003. | |
Other severe adverse effects of clozapine include myocarditis associated with cardiac failure, orthostatic hypotension with circulatory collapse, and rhabdomyolysis (Table).4,7 Leukocytosis and eosinophilia are generally transient and self-limited but may predict agranulocytosis.8,9 The risk of seizure occurs most commonly at dosages greater than 500 mg/d.4
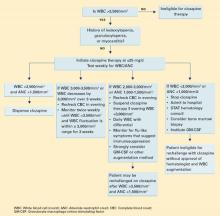
Given these potentially fatal effects, the authors’ treatment guidelines call for potential suspension of clozapine therapy when the WBC is consistently <3,000 mm3 (Algorithm).
CONTINUED TREATMENT: A difficult decision
Ms. G was switched to quetiapine, 100 mg nightly, titrated to 800 mg/d in divided doses.
Approximately 3 weeks later, Ms. G was hospitalized for renewed severe paranoia and command-type auditory hallucinations accompanied by prominent mood lability, avolition, and thought disorganization. During her 7-week hospitalization, she underwent sequential and sometimes overlapping trials of:
- ziprasidone, 160 mg bid
- risperidone, 3 mg bid
- trifluoperazine, 3 mg bid
- haloperidol, 10 mg bid
- divalproex sodium, 500 mg bid
- and carbamazepine, 400 mg bid.
None of these trials significantly improved her psychosis or mood.
At this point, the treating psychiatrists faced a difficult but clear decision: Ms. G was rechallenged on clozapine, 25 mg nightly, titrated again to 300 mg nightly. After she provided informed consent, her WBC was monitored twice daily—morning and evening—for agranulocytosis and to examine WBC patterns. Her average daily WBC counts were 4,200/mm3 in the morning and 5,500/mm3 at night. No physical signs of agranulocytosis emerged.
One week after restarting clozapine, Ms. G became less paranoid and socially more appropriate. Her thought process became increasingly organized, and after 4 weeks she reached her baseline status based upon family reports and the clinician’s CGI Global Improvement rating of 2 (much improved). Her auditory hallucinations resolved, and she was discharged to her family’s care.
Twice-daily blood testing was stopped at discharge. Ms. G continues to take clozapine and receives blood tests every 2 weeks, with no apparent signs of agranulocytosis.
Algorithm Suggested guidelines for managing WBC counts during clozapine therapy
Box
Two treatments for clozapine-dependent agranulocytosis have been described.
- Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a glycoprotein that has been shown to stimulate proliferation of precursor cells in bone marrow and their differentiation into granulocytes and macrophages. Researchers have reported that GM-CSF treatment allows patients to continue taking clozapine after an episode of severe neutropenia.10-12
- Lithium salts have been reported to exploit the natural leukocytosis observed with lithium to counter clozapine-related leukopenia.13 Use of lithium to displace white blood cells has been debated, and anecdotal evidence suggests that combining lithium with clozapine may increase the chance of seizure and neuroleptic malignant syndrome.4 Still, cases reported by Adityanjee and Blier suggest that lithium augmentation is cost-effective and efficacious.14,15
How could Ms. G’s doctors have avoided stopping her clozapine therapy and her subsequent decompensation?
The authors’ observations
Aggressive blood testing and cessation of clozapine therapy are indicated when onset of granulocytopenia and agranulocytosis are suspected. Even with early detection and discontinuation, the chance of infectious disease poses a danger for up to 4 weeks until WBC levels return to normal.4
Given Ms. G’s lack of response to other antipsychotics, however, we had to consider resuming clozapine therapy. Studies have described agranulocytosis management strategies that may allow patients to keep taking clozapine despite low WBC counts (Box).
We also considered the timing of Ms. G’s blood test that showed a WBC count <2,700/mm3. Ahokas16 suggests that evening WBC counts are significantly higher than those taken in the morning and that granulocytes fluctuate in a diurnal pattern. Ms. G’s evening WBC counts were on average 1,300/mm3 higher than morning levels. Allowing for this diurnal variation and comparing evening blood samples could have averted the interruption in Ms. G’s clozapine therapy and prevented relapse in a patient with highly treatment-refractory schizophrenia.
Related resources
- Chong SA, Remington G. Clozapine augmentation: safety and efficacy. Schizophr Bull 2000;26:421-40.
- Emsley R, Oosthuizen P. The new and evolving pharmacotherapy of schizophrenia. Psychiatr Clin North Am 2003;26:141-63.
- Barnas C, Zwierzina H, Hummer M, Sperner-Unterweger B, Stern A, Fleischhacker WW. Granulocyte-macrophage colony-stimulating factor (GM-CSF) treatment of clozapine-induced agranulocytosis: a case report. J Clin Psychiatry 1992;53:245-7.
Drug brand names