Imaging and radiation exposure
With the advent of CT scans in the 1970s, psychiatrists gained a new method of investigating potential structural CNS pathology in patients presenting with psychiatric symptoms. The dramatic increase in CT scan use in recent years and resulting radiation exposure is responsible for 1.5% to 2% of all cancers in the United States.12,13 Certainly, physicians must balance the advantage of early detection of brain lesions with cost-effectiveness and exposure to radiation.14
There is no consensus regarding use of brain imaging in a patient who presents with new-onset psychiatric symptoms. Certainly, patients with localizing neurologic deficits or symptoms of increased intracranial pressure should undergo brain imaging. As for psychiatric patients without neurologic findings, Filley and Kleinschmidt-DeMasters15 provide recommendations based on their 1995 case series, and other authors have recommended imaging for patients age ≥4016 vs ≥5017,18 who present with atypical mental status changes.
OUTCOME: Scan, then surgery
Ms. D’s head CT reveals a large right-sided temporoparietal low-density lesion with 8-mm left lower midline shift (Figure). She undergoes a right temporal craniotomy with resection of the mass, which is confirmed by surgical pathology to be a glioblastoma multiforme World Health Organization grade 4 tumor. Postoperative MRI shows evidence of infarction in the right posterior cerebral artery distribution and residual tumor is identified on follow-up imaging. Ms. D is referred to radiation oncology, where she receives a prognostic median life expectancy of 14 months with radiation and temozolomide treatment.19
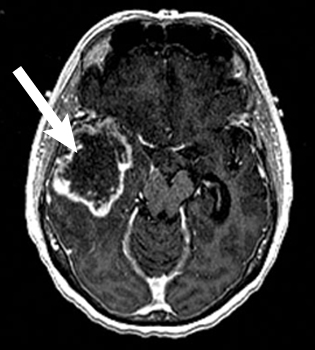
Figure: Ms. D’s MRI results
MRI with contrast shows a large right temporal heterogeneous mass consistent with glioblastoma multiforme
The authors’ observations
Glioblastoma is a rare cancer that comprises 25% of all malignant nervous system tumors.20 It is associated with a poor prognosis, with a <30% relative survival rate for adults at 1 year and 3% at 5 years.20 Headaches, seizures, motor weakness, and progressive neurologic deficits are common symptoms of glioblastoma at diagnosis.20 Ms. D was offered the standard of care treatment for a high-grade glioma, including surgical resection followed by concomitant external-beam radiotherapy and chemotherapy.21
Consider structural brain lesions in patients who present with neurobehavioral symptoms, although most of these patients will be diagnosed with a primary psychiatric disorder. Ms. D had a known psychiatric disorder that predated the onset of neurologic symptoms and diagnosis of a rare brain cancer. Before she developed neurologic signs, Ms. D experienced symptoms uncharacteristic of her previous depressive episodes, including olfactory hallucinations, that provided an early indicator of a CNS lesion. Consider brain imaging in patients of any age who do not respond to medications targeting the presumed psychiatric diagnosis to ensure that insidious brain tumors are not missed (Table 1).15
Table 1
When to order neuroimaging for psychiatric patients
| Patient’s age | Most common types of brain tumor | MRI vs CT | Indications to image |
|---|---|---|---|
| ≥40 years | Metastases High-grade gliomas Meningiomas | Roughly equivalent for imaging common tumor types. Base on cost, availability, and relative patient contraindications | New-onset cognitive or emotional dysfunction. Patient is not responding to appropriate pharmacotherapy for psychiatric diagnosis |
| <40 years | Low-grade astrocytomas Oligodendrogliomas | MRI preferred | New-onset cognitive or emotional dysfunction with associated somatic symptoms (headache, nausea, vomiting, papilledema, seizures, or focal deficits). Patient is not responding to appropriate pharmacotherapy for the psychiatric diagnosis |
| Source: Reference 15 | |||
Compared with cerebrovascular lesions, neoplasms are more difficult to clinically correlate with their anatomic location. Neurobehavioral symptoms are more frequently associated with tumors originating in the frontal lobe or temporolimbic regions of the brain. The 3 types of frontal lobe syndromes are dorsolateral, orbitofrontal, and medial-frontal (Table 2).15 Temporolimbic tumors may present with hallucinations, mania, panic attacks, or amnesia. A meta-analysis found a statistically significant association between anorexia and hypothalamic tumors.22 Reports of neuropsychiatric symptoms that respond to pharmacologic treatment further confound the clinical picture.16
Table 2
Frontal lobe syndromes
| Syndrome | Characteristics |
|---|---|
| Dorsolateral | Deficits in executive functioning, including organization and behavior planning |
| Orbitofrontal | Prominent disinhibition |
| Medial-frontal | Apathy, abulia |
| Source: Reference 15 | |
It is uncommon for a patient with a long-standing mood disorder to develop a primary brain cancer. However, Ms. D’s case serves as an important reminder to consider medical comorbidities in our aging psychiatric population. In particular, a patient who develops unusual symptoms or does not respond to previously effective treatments should be more closely examined and the differential diagnosis broadened.
Related Resources
- MD Anderson Cancer Center. Brain tumor videos and podcasts. www.mdanderson.org/patient-and-cancer-information/cancer-information/cancer-types/brain-tumor/videos-and-podcasts/index.html.
- Braun CM, Dumont M, Duval J, et al. Brain modules of hallucination: an analysis of multiple patients with brain lesions. J Psychiatry Neurosci. 2003;28(6):432-449.

